AI in EHRs: Potential and Use Cases

As indispensable as EHRs have become, they are often sources of frustration for healthcare professionals. Complaints around usability, time-consuming data entry, and systems designed more for billing than clinical decision-making are widespread. AI-enhanced EHR systems hold immense potential for streamlining workflows, improving data analysis, and supporting better decision-making.
This piece explores how AI in EHR works and what outcomes healthcare professionals are witnessing. We'll break down real-world cases of companies excelling at AI development for healthcare and how their advances could revolutionize the industry.
The Need to Improve Electronic Health Records
Medical errors remain a critical concern, often stemming from insufficient or incomplete patient information available to doctors during clinical decision-making. A landmark report from the Institute of Medicine, "To Err is Human", highlighted the gravity of this issue, revealing that between 250,000 and 440,000 deaths per year in the United States are attributable to medical errors. These preventable mistakes are now regarded as the third leading cause of death in the country. Alarmingly, research suggests that 76% of these errors could have been mitigated through the adoption of advanced systems. This has consequently driven the global implementation of Electronic Health Records systems.
The adoption of EHRs marks a pivotal development in the digitization and modernization of the healthcare industry. Over 96% of hospitals and 89% of private practice physicians in the U.S. rely on EHRs, making these systems a pivotal component of healthcare operations. On average, physicians spend 4.5 hours daily navigating EHR platforms, with many dedicating additional time outside clinic hours to finalize digital paperwork.
However, the rapid expansion of health-related data, while beneficial, has also introduced a new challenge: effectively processing and extracting actionable insights from this massive pool of medical information has become a pressing priority in maximizing the efficiency of EHR systems. So, today's EHRs are no longer about digitizing paper-based medical records. It is about unlocking the potential of Big Data and empowering healthcare providers.
AI in EHR
Data management has always been a challenge for healthcare providers, primarily due to the "4 Vs" of big data:
- Velocity (rapidly growing data),
- Volume (enormous quantities of information),
- Variety (structured and unstructured data), and
- Veracity (ensuring data accuracy).
AI excels at handling large-scale data. Industry giants have already recognized its potential. The market cap for AI-enhanced EHRs is projected to reach around $52 billion by 2033. Which tech subsets exactly are about to make this happen?
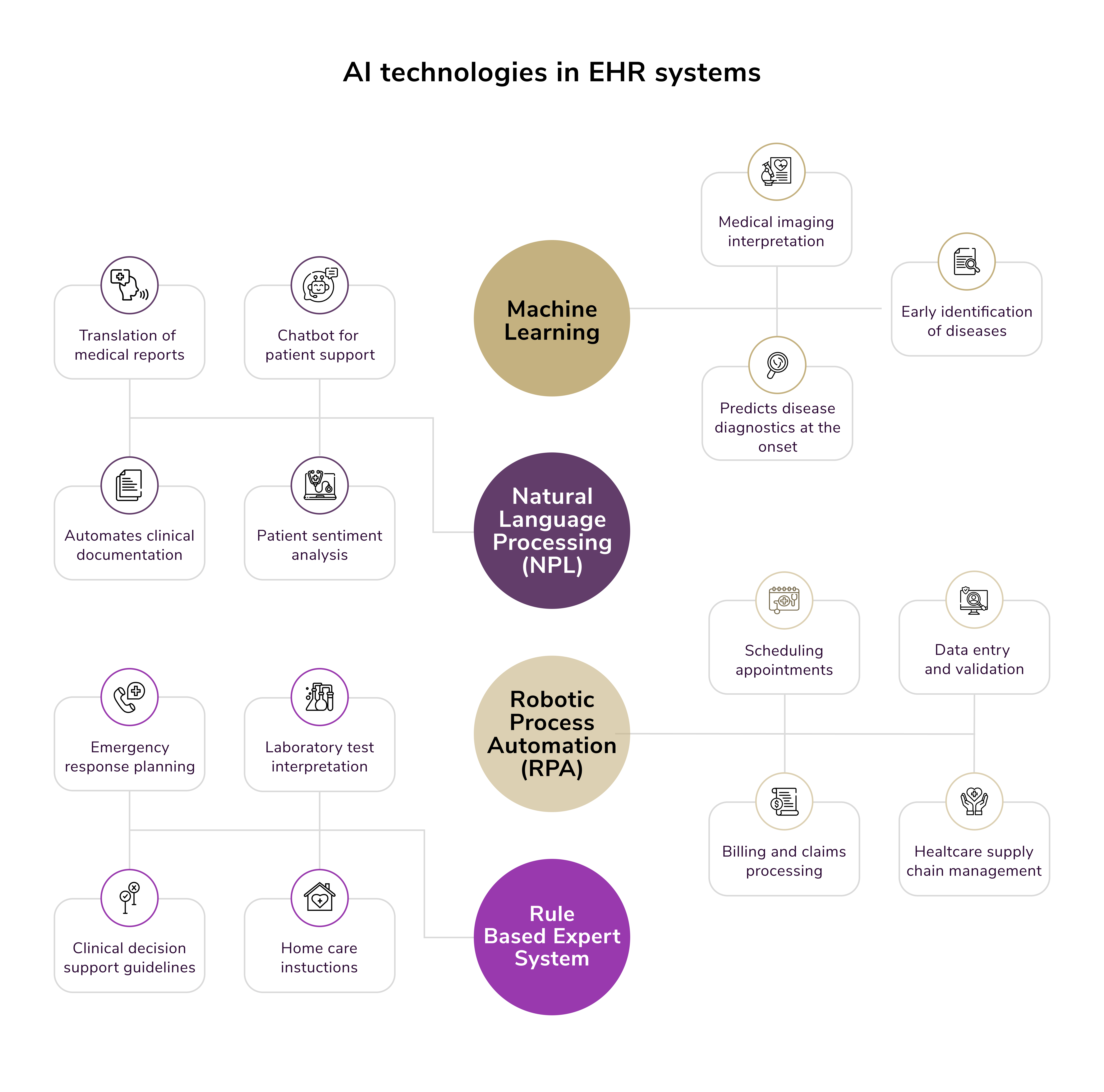
NLP
Unstructured data (clinical notes, discharge summaries, and patient feedback) accounts for over 80% of healthcare data. Natural language processing makes sense of this data, transforming it into actionable insights.
- Streamlining documentation: NLP converts complex clinical notes into structured formats like ICD-10 and CPT codes. This reduces documentation time by up to 40%, saving doctors an estimated 3.5 hours per shift to focus on patients.
- Extracting insights: Tools like Amazon Comprehend Medical and IBM Watson Health are improving the accuracy of coding by identifying crucial data, including diagnoses, allergies, and medications.
- Ambient listening tools: These record and transcribe clinician-patient encounters in real time, seamlessly entering the data into the patient's EHR. Physicians can also dictate notes directly to such systems.
Note: According to AI in Healthcare, AI can evaluate user interaction patterns within EHR interfaces to pinpoint usability challenges, allowing developers to design more user-friendly systems that cater to specific needs. This approach helps reduce user frustration and encourages broader adoption of EHR systems among healthcare professionals.
ML
ML plays a critical role in analyzing vast datasets to uncover patterns that can improve care and operational processes. It strengthens healthcare professionals' abilities to enhance patient care and creates a safer and more efficient healthcare environment.
- Anomaly detection: ML flags unusual patterns in patient data. For instance, identifying irregularities in heart rate data could prompt further investigation and prevent complications. Meanwhile, reasoning in AI can help recommend personalized treatment plans.
- Predictive problem solving: Algorithms use historical data to predict potential issues like equipment failures, saving time, and improving resource allocation. ML models can also forecast risks such as sepsis or heart failure, allowing for early intervention. For example, the University of Chicago Medicine reduced ICU transfers by 20% using ML-based early warnings.
- Disease detection: Tools like Northwell Health's iNav identify diseases like pancreatic cancer early by analyzing MRI and CT scans, halving the time from diagnosis to treatment and improving survival rates.
RPA
Administrative inefficiencies burden many healthcare organizations, but RPA is providing much-needed relief by automating repetitive tasks.
- Reducing administrative costs: Hospitals employing RPA cut admin costs by up to 50%, potentially saving the industry $150 billion annually.
- Streamlining workflows: RPA handles processes like patient scheduling, insurance claims, and billing, allowing healthcare professionals to focus on direct patient care.
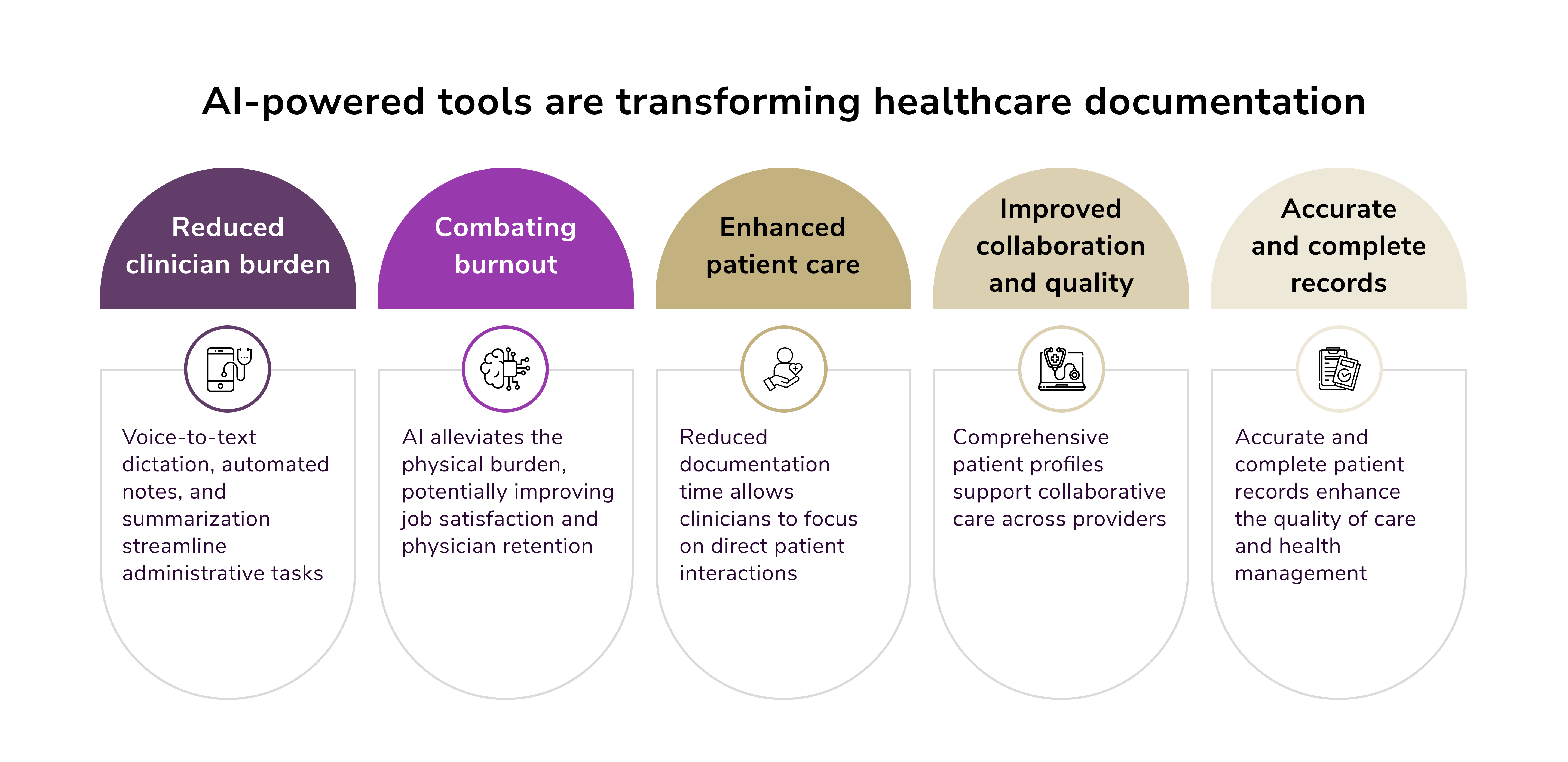
Benefits of AI in EHR Systems
At its best, EHR AI represents a collaboration between cutting-edge technology and human expertise. The goal isn't to replace clinicians but to empower them. By handling repetitive, time-heavy, and data-intensive tasks, AI frees up medical professionals to focus on what they do best: delivering compassionate, personalized care to their patients.
The study by researchers at Stanford University shows that AI can be utilized effectively to summarize clinical text. Large language models analyze and condense a wide range of clinical documents, including radiology reports, progress notes, and even patient questions. The results were groundbreaking:
- Accuracy: Physicians who evaluated summaries generated by LLMs rated many of them as being as good as or better than human-written summaries. Impressively, doctors judged AI summaries to be "superior" 36% of the time.
- Reduced errors: AI models were found to introduce fewer errors or "fabricated information" compared to human-generated summaries. This demonstrates that, with proper training and adaptation, AI tools in EHR can reduce inaccuracies that could lead to potential patient harm.
The Stanford study tested eight large language models, adapting them specifically for clinical text summarization. These LLMs were evaluated using a rigorous process by a panel of 10 practicing physicians who rated summaries based on completeness, correctness, and conciseness. The outcomes demonstrated AI's exceptional potential. Not only did the models perform exceptionally well, but they also proved reliable in reducing errors, a perennial concern in medical settings.
Importantly, developers are continuously refining these models to bring them closer to real-world clinical applications. External financial support from institutions like Microsoft Azure, OpenAI, and the National Institute of Health suggests widespread interest in bringing such technologies to scale.
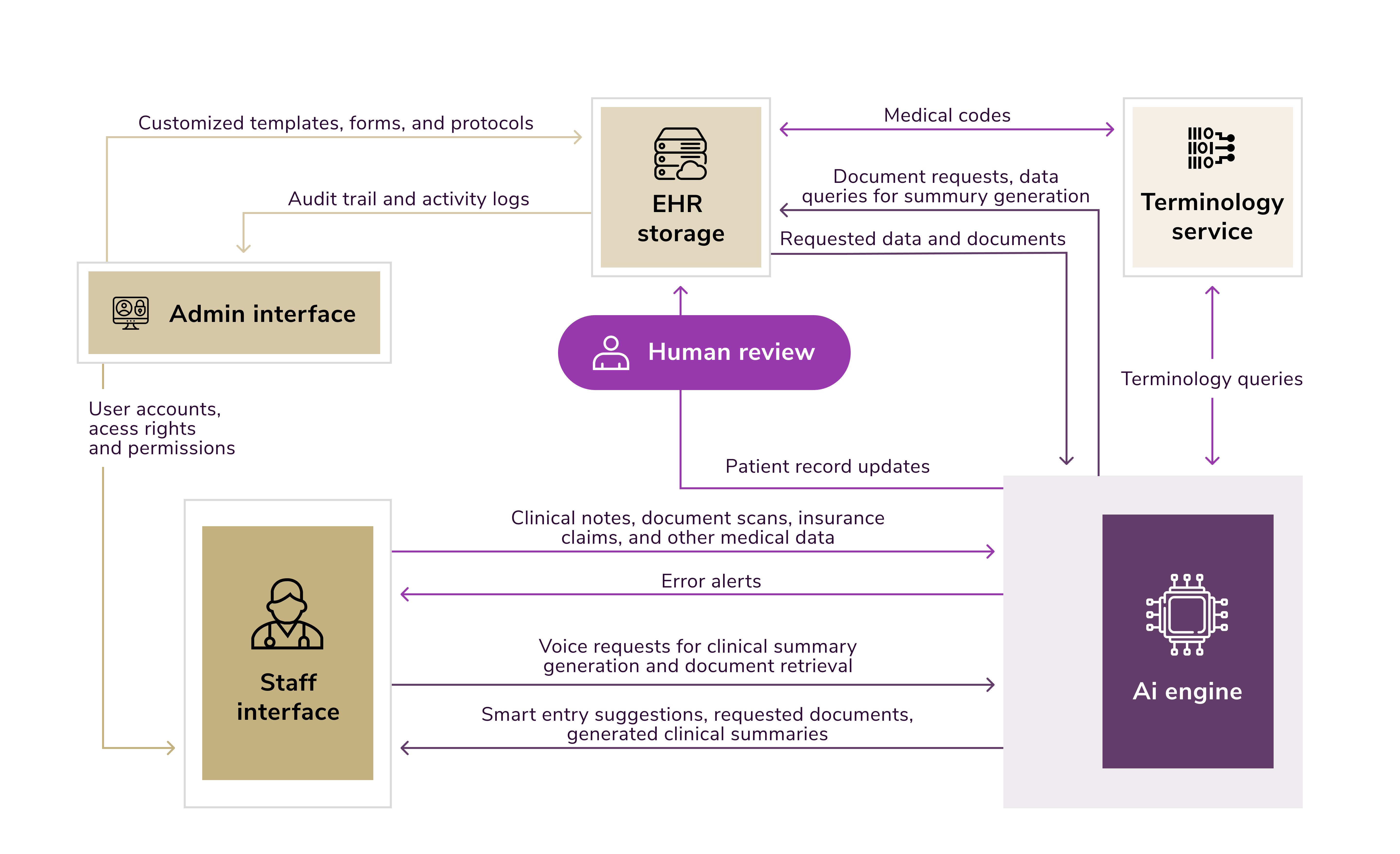
AI in EHR Automation
AI and RPA technologies are uniquely positioned to address inefficiencies and bottlenecks in managing EHRs. Healthcare organizations using AI to improve electronic health records can improve data accuracy, reduce operational costs, and ultimately elevate the level of care provided.
Now, let's look at three pivotal areas where AI in EHR automation can make a significant impact.
Data Processing
Healthcare orgs handle large volumes of unstructured data, ranging from patient histories and treatment plans to X-ray images and clinical notes. Manually extracting actionable information from these documents is time-consuming and prone to errors.
AI-driven tools like OCR and NLP extract critical data from unstructured formats. For instance:
- OCR reads scanned documents or images, like handwritten prescription forms, and converts them into structured, editable text.
- NLP interprets clinical text to identify relevant data, such as diagnoses or medications.
- ML algorithms help classify and identify appropriate information in seconds, helping healthcare professionals streamline access to medical data stored in EHRs.
With these capabilities, AI EHR solutions ensure that vital medical records are available within seconds, eliminating the need for inefficient manual processes.
Report Management
Healthcare workflows involve maintaining various records, including patient appointments, billing documents, and insurance claims. Managing and consolidating data from legacy systems, while maintaining accuracy, burdens healthcare professionals.
Intelligent bots collect, compile, and store data all in one place by integrating with existing legacy systems. AI updates information in real-time, resolving delays in insurance documentation or payment processing. Medical professionals can access accurate records instantly, helping doctors make informed clinical decisions faster.
Regulatory Compliance
Rigorous regulations govern the healthcare industry to ensure data security and privacy. Compliance requirements like HIPAA (Health Insurance Portability and Accountability Act) demand meticulous record-keeping, leaving healthcare organizations vulnerable to audits if processes aren't airtight.
AI algorithms validate patient records by checking for inconsistencies or missing information, ensuring compliance risks are mitigated promptly. Meanwhile, RPA tools automatically track, record, and categorize compliance-related activities into structured formats. So, sensitive healthcare data remains protected and accessible only to authorized personnel.
GenAI in EHR
Generative AI, and more specifically LLMs, have demonstrated remarkable capabilities in understanding, processing, and generating human language. When trained on EHR data, these advanced AI models offer unprecedented precision and efficiency in handling the diverse and complex demands of modern healthcare systems. Below, we delve deep into how exactly GenAI works for EHRs and what value it delivers.
Named Entity Recognition (NER)
NER focuses on extracting structured data from unstructured text. It identifies and classifies specific entities such as diagnoses, medications, and medical conditions within clinical records.
- Streamlined medical history: AI models, such as BERT and GPT-based systems, extract critical details from patient records, creating a comprehensive view of their medical history.
- Social determinants of health: NER isn't limited to clinical information. It also extracts data on social determinants like employment or access to healthcare services, enabling a holistic approach to patient care.
Information Extraction
Information extraction extends beyond NER by identifying relationships between entities and events. This deeper understanding helps to map out sequences of medical events and build actionable knowledge.
- Specialized solutions: CancerBERT model extracts highly specific pieces of information, such as phenotypes or relational data, from clinical text.
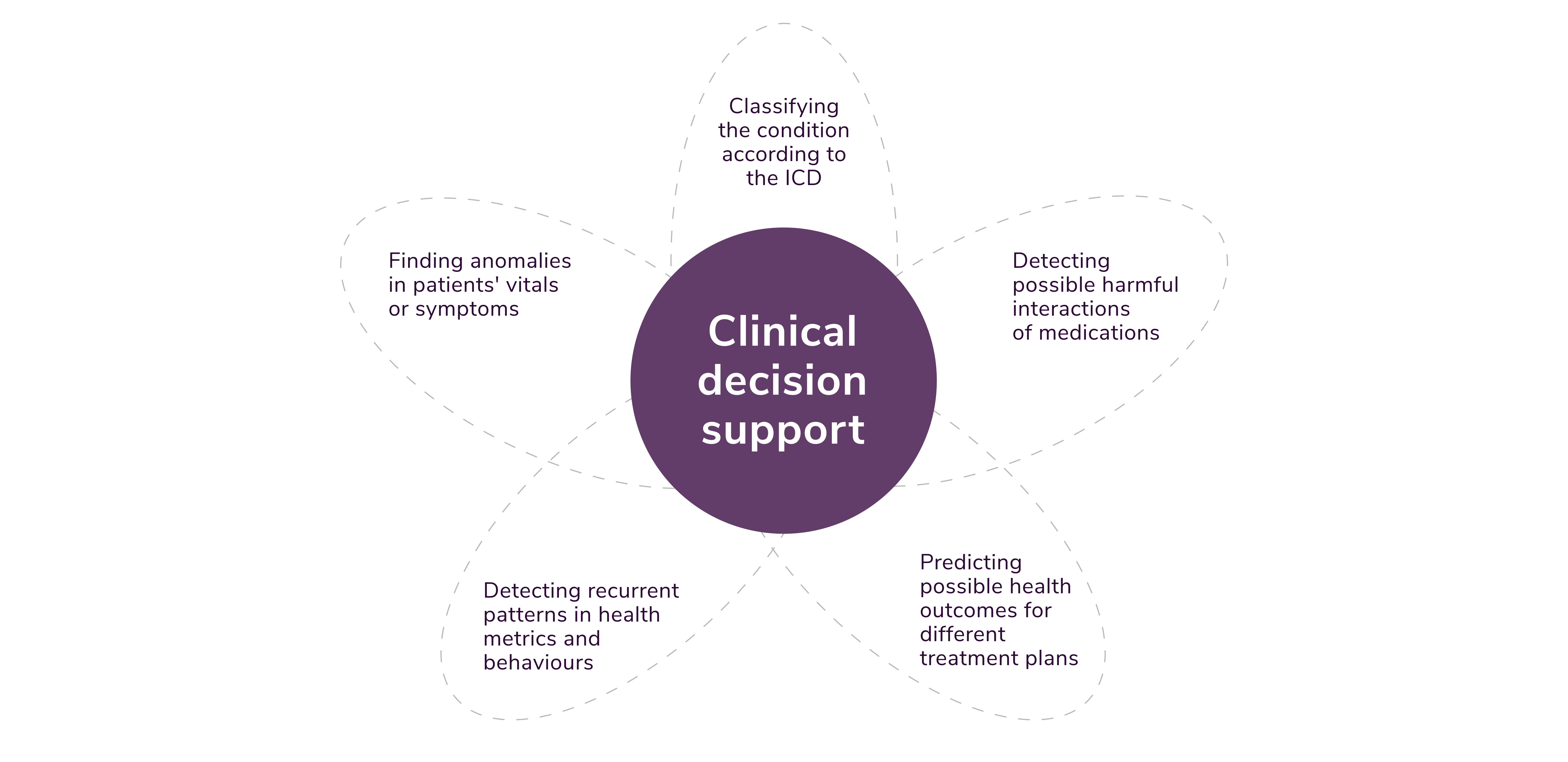
- Improved clinical decision support: These extracted insights feed into AI-powered decision support systems to guide physicians during diagnoses or treatment planning.
Text Summarization
Consider the volumes of clinical notes, discharge summaries, and lab results generated daily. Text summarization condenses these data sources into concise, patient-friendly, or doctor-focused summaries.
- Efficiency in documentation: Fine-tuned models like BERT and BART condense dense information into actionable insights, helping doctors spend less time documenting and more time on patient care.
- Enhanced communication: Summaries are easily understood by patients, improving their engagement with their healthcare plans.
Text Classification
Text classification assigns data to specific categories, such as prescription details, adverse drug reactions, or chronic disease classifications.
- Efforts in automation: AI models such as BioBERT and ClinicalXLNet excel at categorizing disorder types or mapping ICD codes.
- Enhanced analytics: Well-classified data sets the stage for advanced analytics, aiding predictive and preventive care strategies.
Conversational Agents
Conversational agents represent the human-like frontiers of AI in healthcare. These systems assist both patients and medical professionals.
- Patient interaction: AI-powered agents handle routine patient inquiries, freeing medical staff from repetitive communication tasks.
- Clinician support: Advanced LLMs like GPT-4 provide physicians with quick summarizations, propose diagnostics, and highlight overlooked data in patient histories.
Note: AI can bring many positive changes to EHRs; there is no doubt about that. However, this innovation comes with its share of controversies. Supporters argue for its benefits in improving accuracy, efficiency, and equity. Meanwhile, critics raise ethical concerns about data privacy, informed consent, and algorithmic bias. Ultimately, the integration of AI into EHR systems is not an "if," but a "when." By addressing challenges methodically and inclusively, the healthcare industry can ensure AI enhances, not compromises, patient care.
Application of AI in EHR
To better understand how EHRs can be enhanced by AI, take a look at how the pioneers on the market are employing it. Below are some real-world examples of tools and systems and how they work.
Streamlining Documentation
Managing patient records has long been one of the most time-intensive tasks in healthcare. AI offers a way to optimize this process, allowing healthcare providers to focus more on patient care and less on administrative burdens. For instance, AI can identify patterns in previous entries to autocomplete common fields, ensuring standardized and accurate documentation. Ambient listening tools can convert physician notes into structured EHR entries, saving critical time for busy professionals.
A good example is Nuance Dragon Medical One. It is a voice recognition tool that transcribes physician-patient conversations into structured EHR notes. It thus reduces the time physicians spend on manual data entry.
Another exemplary tool is Praxis EMR. Unlike template-based EHR systems, Praxis leverages AI-driven concept processing technology. It learns physicians' workflows and adapts, making charting quicker and reducing redundant tasks. This feature can greatly reduce physician burnout, as it will make the computer conform to the provider, not the other way around.
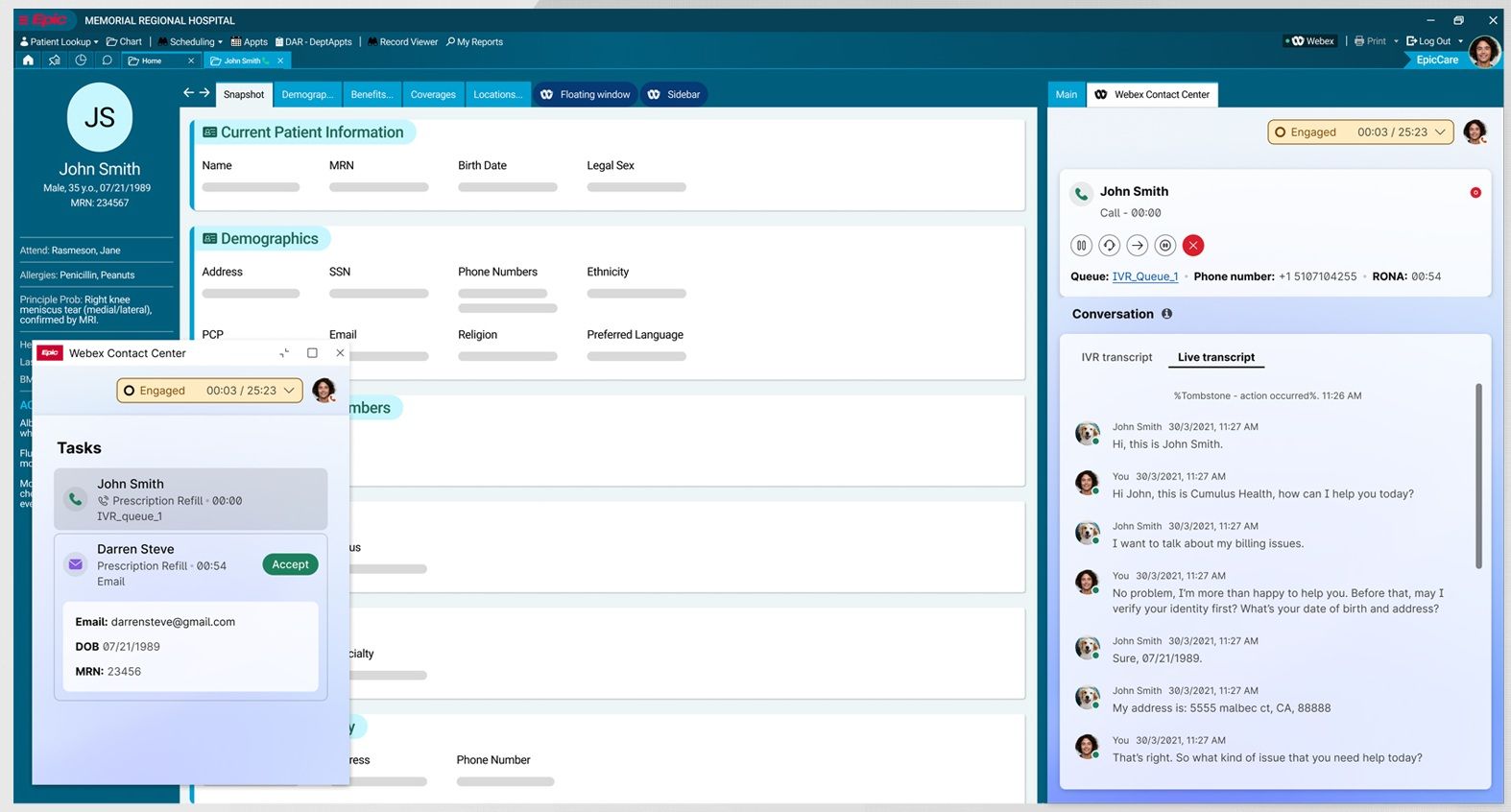
It would be wrong not to mention Epic. It is a prominent provider of healthcare software solutions, specializing in electronic health records (EHR). Trusted by over 600,000 physicians and millions of professionals, Epic supports access to more than 305 million patient records, representing 60% of the U.S. population. The latest Epic integration with Webex Contact Center equips agents with a robust and intuitive communication platform.
Detecting Errors in EHRs
Errors in EHRs can range from minor typos in patient records to more severe issues like medication mismatches or incorrect dosages. Through ML algorithms, NLP, and pattern recognition, AI tools can flag discrepancies, unusual patterns, and potential risks with remarkable accuracy.
MedAware, for instance, uses ML to analyze data from millions of patient records. Its primary goal? To detect and prevent medication-related errors that could harm patients.
Here are some of its standout features:
- Medication safety monitoring: identifies anomalies, such as prescribing blood thinners to a patient with a history of hemorrhaging.
- Patient context recognition: ensures prescriptions align with each individual's unique needs.
- Real-time alerts: sends alerts to physicians immediately when a potential issue is detected.
MedAware has already proven its value in numerous healthcare settings. One notable example comes from a study published in the Journal of the American Medical Informatics Association (JAMIA). MedAware detected 75% of significant errors, a substantial improvement over the detection rates of traditional clinical decision support tools.
Detecting and Preventing Fraud
Fraud in EHR is a pressing issue in the healthcare industry. From upcoding and phantom billing to duplicate claims, these deceitful practices cost the U.S. healthcare system billions of dollars every year. Below, we'll take a closer look at four AI-driven fraud detection tools designed to combat EHR fraud and save the healthcare industry from unnecessary losses.
The Sherlock System, developed by MediBuddy, stands out as one of the frontrunners in AI-based fraud detection for healthcare reimbursements. Sherlock employs ML and data analytics to analyze billing claims in real time. The system searches for patterns and anomalies that indicate potential fraudulent activities. For example, it can detect:
- Duplicate claims: instances where the same medical procedure has been submitted for reimbursement more than once.
- Manipulated documentation: irregularities in patient records that might suggest intentional tampering.
- Pricing errors: charges that deviate greatly from standard pricing guidelines.
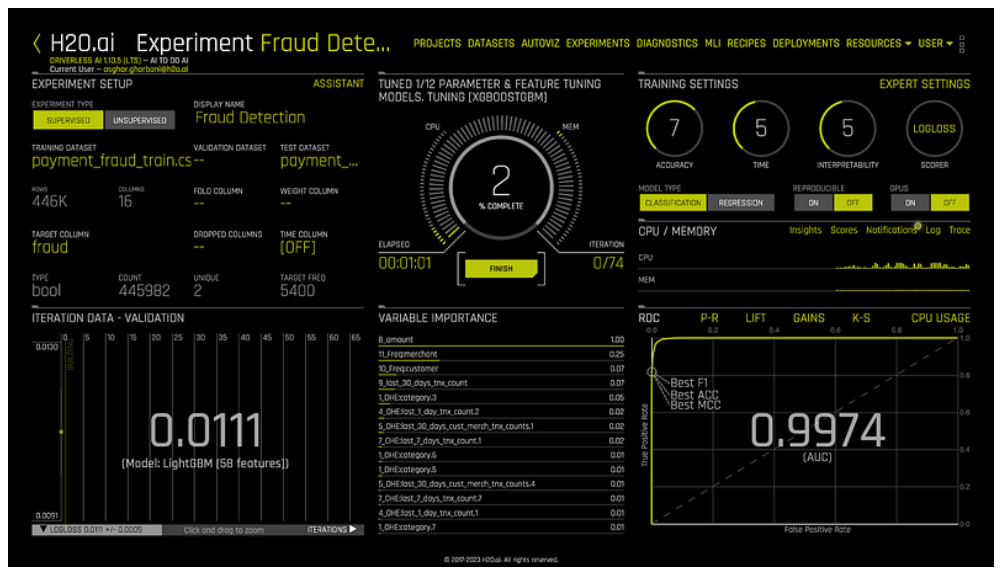
H2O.ai's technology leverages anomaly detection algorithms to analyze vast amounts of EHR and claims data. It enables faster, more accurate detection of widespread fraud. The top two gains for providers are:
- Reduced false positives, allowing investigators to focus only on genuine cases.
- Enhanced scalability, accommodating growing datasets seamlessly.
Here's an example of H2O.ai's fraud detection model:
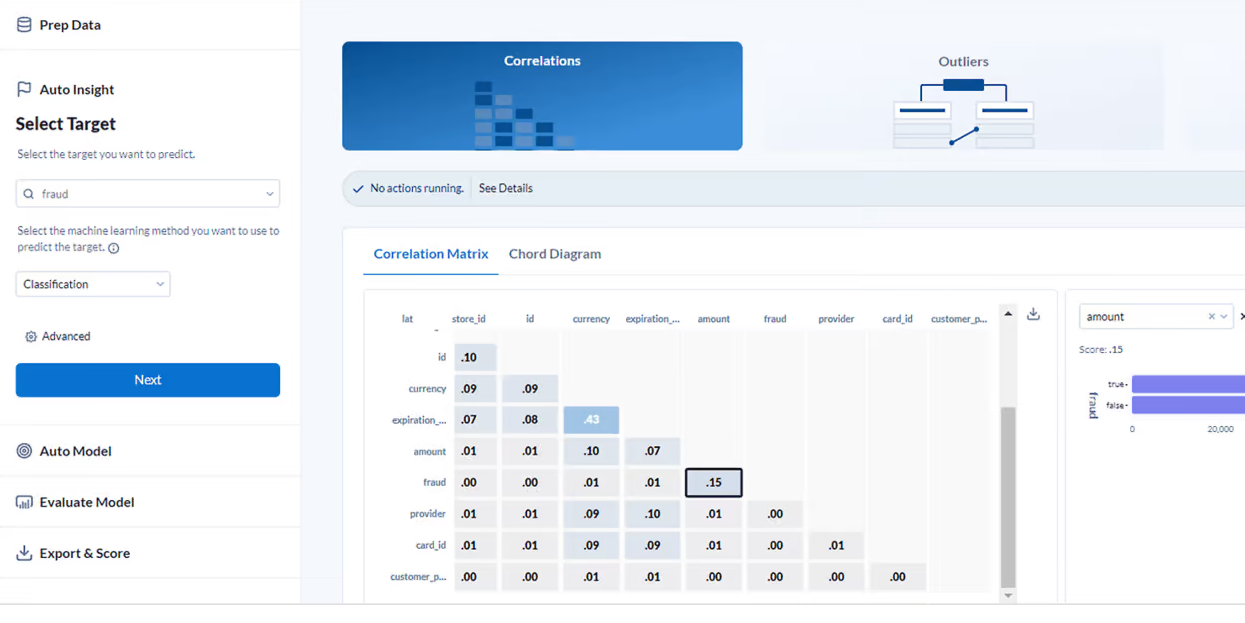
Alteryx, another great tool, combines data analytics with machine learning to tackle EHR fraud, making it an indispensable tool for healthcare administrators. The platform simplifies the complexities of fraud detection by providing:
- Predictive modeling: it forecasts potentially fraudulent patterns based on historical claims data.
- Geospatial analysis: identifies suspicious billing activities, such as medical claims submitted from locations far from a patient's residence.
- Customizable workflows: tailored fraud mitigation plans that fit the unique needs of different organizations.
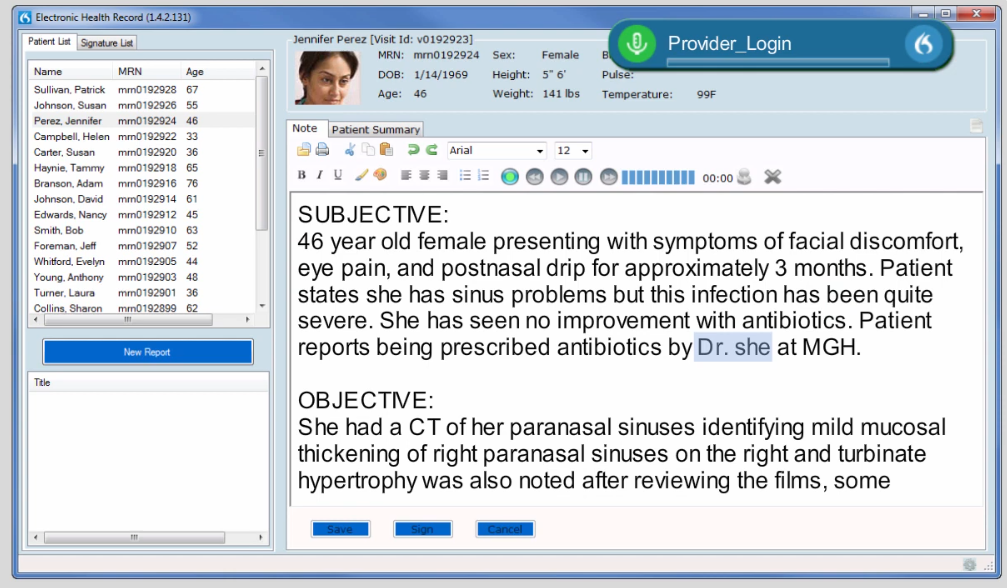
Generating Clinical Notes
Efficient documentation is the backbone of modern healthcare. Yet it remains one of the most time-consuming tasks for medical professionals.
Trusted by over 80,000 physicians, Sunoh.ai is an AI medical scribe that listens to natural conversations between healthcare providers and patients and converts them into high-quality clinical notes. It seamlessly integrates with EHR systems to streamline documentation and elevate patient care.
Sunoh.ai starts by actively listening to patient-provider interactions, accurately capturing everything said during appointments. Using advanced voice recognition and AI, it then creates a detailed transcript of the conversation. The system organizes the transcript into Progress Note sections like Chief Complaint, History of Present Illness, or Assessment and Plan.
Tali AI is another remarkable solution for automating clinical notes through intelligent scribing capabilities. Designed with an emphasis on efficiency and customization, it enables healthcare providers to shift their focus back to patient care without worrying about tedious administrative tasks.
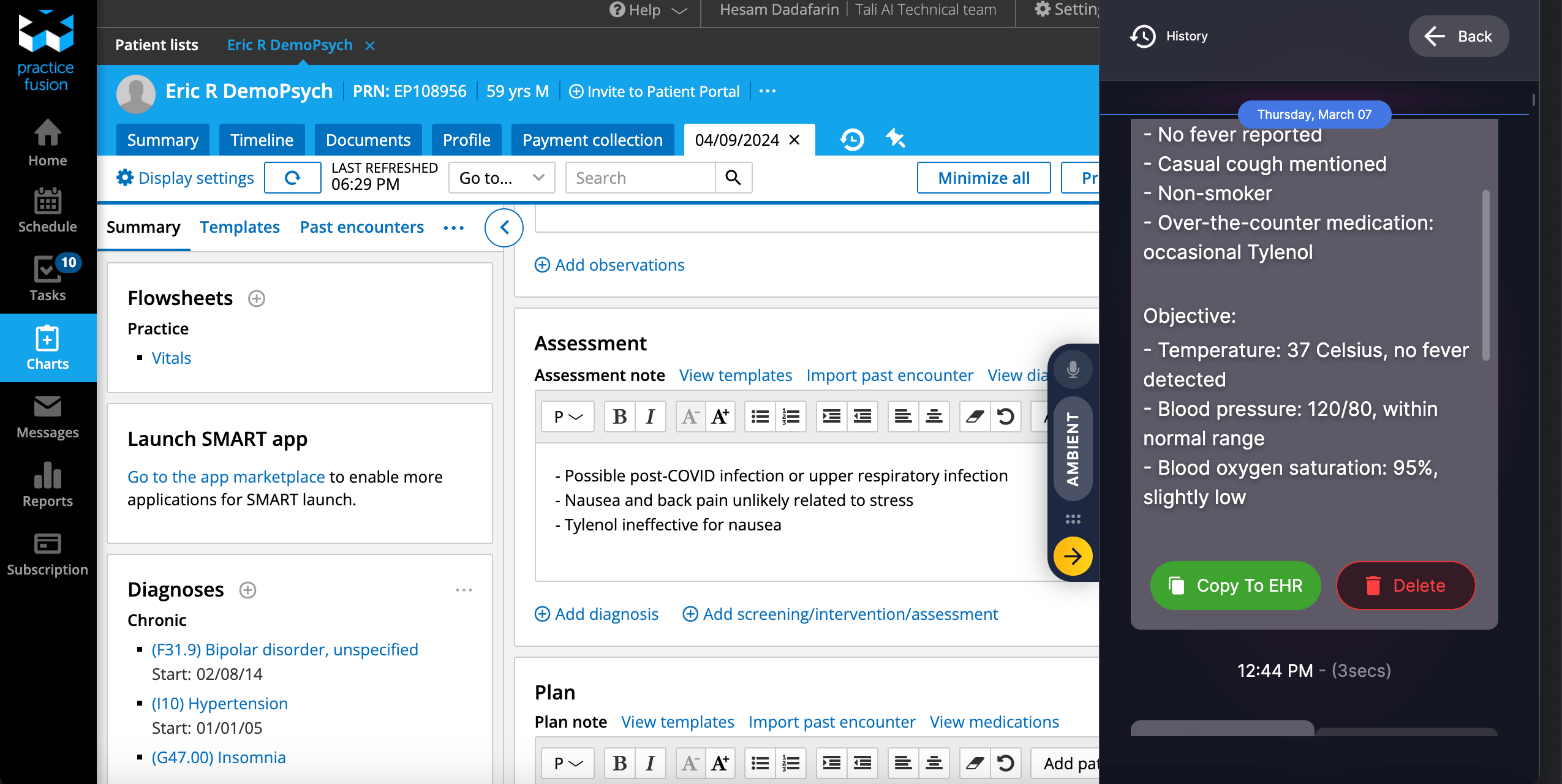
Tali listens to patient interactions to generate accurate clinical notes automatically. These notes can be reviewed, edited, and directly integrated into EHR systems.
A cutting-edge tool from Amazon Web Services, AWS HealthScribe blends generative AI with advanced speech recognition to deliver high-precision clinical notes. This HIPAA-eligible solution is built for healthcare vendors looking to speed up note-taking processes while maintaining data security.
Here's an example of the app experience that healthcare developers can provide users with AWS HealthScribe.
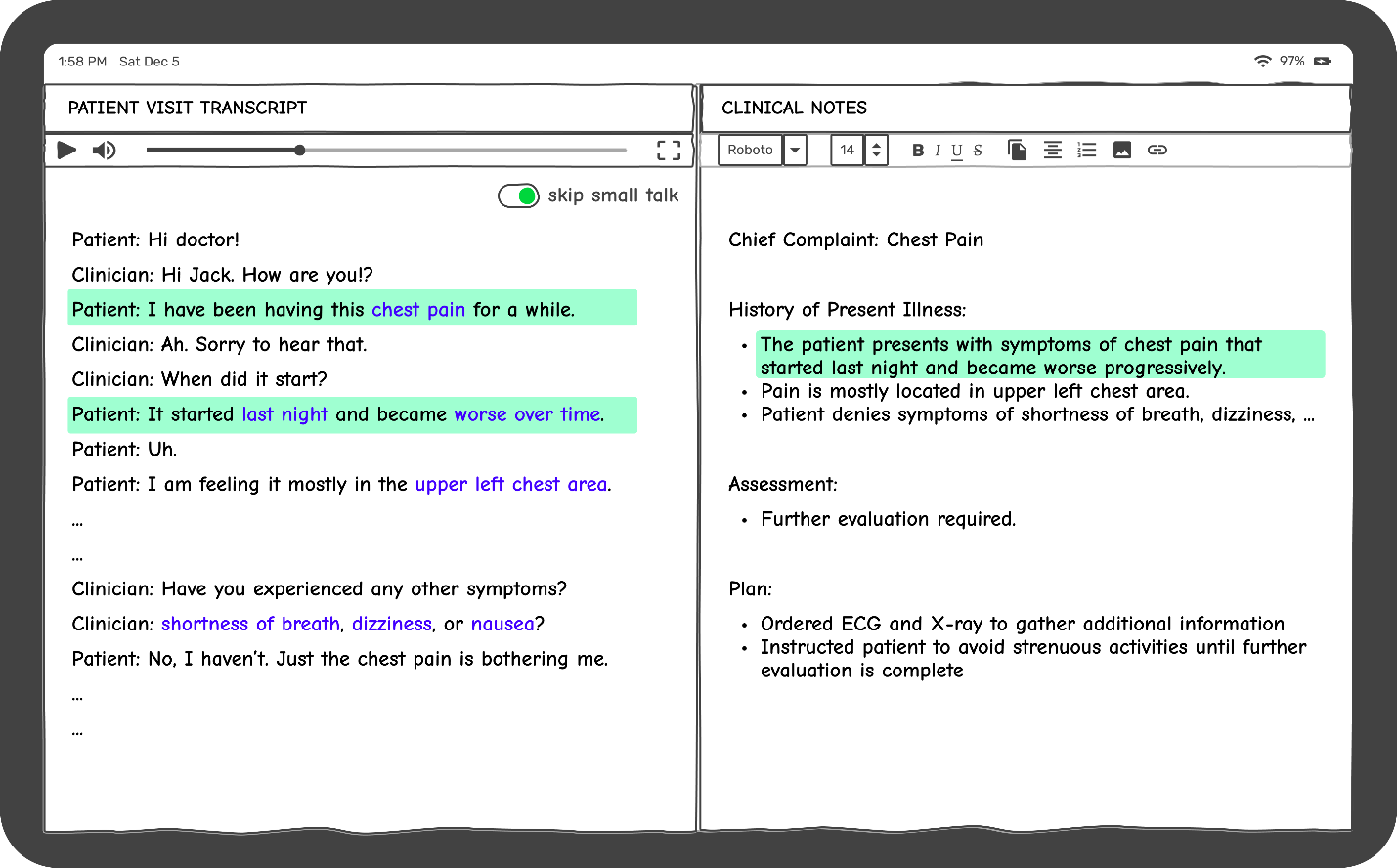
According to AWS, "HealthScribe is designed responsibly, with each AI-generated summary sentence linked back to the consultation transcript.”
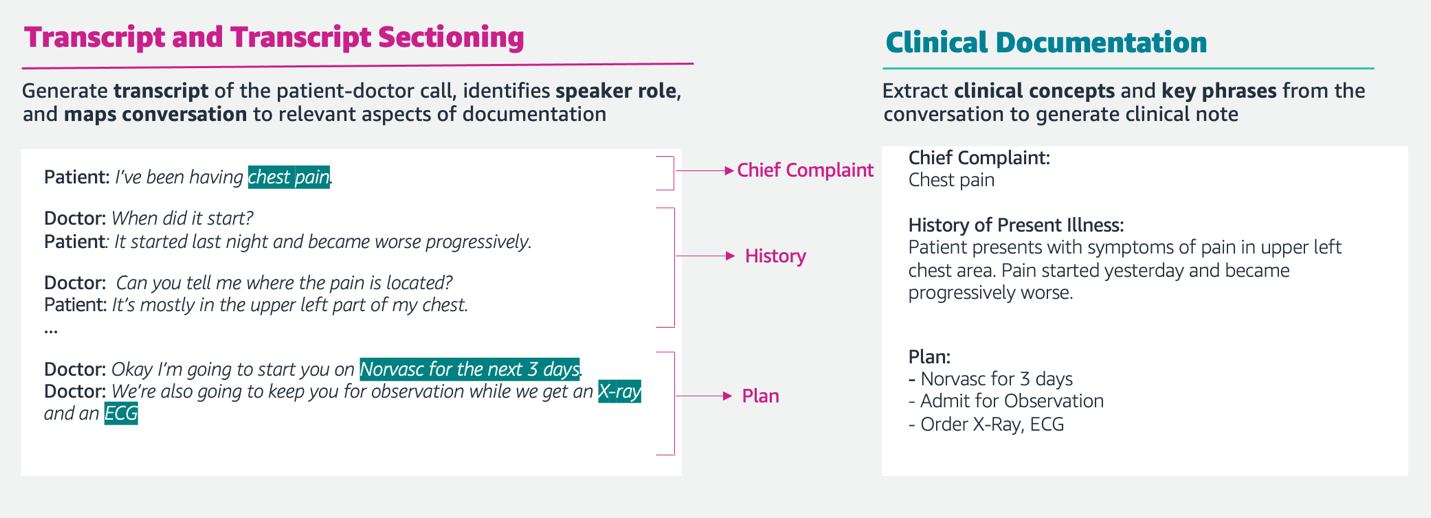
AWS HealthScribe creates structured clinical notes by analyzing patient-provider conversations. It organizes information into relevant sections like Chief Complaint and Treatment Plan. The system identifies and extracts medical conditions, treatment plans, and medication data from transcriptions, ensuring accuracy and completeness.
Improving Population Health Management
Population health management is a proactive approach to improving health outcomes across a specific group of people. Leveraging EHRs has been a game-changer for providers, offering centralized patient data that supports better care coordination. However, as the volume and complexity of patient data grow, healthcare organizations are turning to AI to unlock the full potential of EHRs.
Note: Why is AI essential for leveling up population health management? See, the approach involves assessing and improving the health outcomes of specific groups by identifying trends, risks, and care gaps. The goal is simple yet complex—to shift healthcare from reactive to proactive. AI's predictive analytics capabilities are invaluable in this space.
We've already mentioned Epic Systems in this piece. And here we go again. The thing is, Epic is a giant in the EHR space. The tool has made significant strides in incorporating AI-driven tools to improve population health. With solutions like Healthy Planet, Epic empowers providers with real-time analytics and risk stratification tools.
Here's how it works:
- Epic's tools pull data from a range of sources, including claims, labs, and external networks, to provide a full picture of patient health.
- AI evaluates a patient's risk level using predictive algorithms, helping care teams prioritize high-risk individuals quickly.
- Providers receive alerts for preventive care, such as overdue health screenings or vaccinations.
- Epic's registries and reporting tools enable care teams to monitor outcomes and ensure adherence to best practices.
Here are the expected outcomes:
- Reduced hospital readmission rates by proactively identifying at-risk patients.
- Improved chronic disease management for conditions, such as diabetes and heart failure, by enabling timely interventions.
- Enhanced provider workflows by minimizing duplicate testing and redundant procedures, cutting costs and time.
Convolutional Neural Networks and Their Role in Imaging
CNNs, a type of deep learning algorithm, are at the core of AI's success in medical imaging. Why are CNNs so effective? They mimic the human brain's visual processing abilities, allowing the algorithm to:
- Identify edges, textures, and shapes in images (e.g., identifying tumors or fractures).
- Learn and improve over time using large datasets of medical scans.
- Distinguish between subtle differences in normal and pathological tissues beyond human capabilities.
While CNNs and other AI models provide impressive imaging insights, their true potential is unlocked when paired with patient context. That's where EHR systems come in. Integrating AI-powered imaging data with an EHR system provides clinicians with a comprehensive view of the patient's health. For example:
- A physician examining an X-ray flagged for bone density loss can instantly see prior bone density scores and medications affecting bone health within the EHR.
- Lab results appended to an AI-generated chest CT report may confirm suspicions of an infectious disease, streamlining the path toward targeted therapy.
Zebra Medical has developed AI algorithms that analyze a diverse range of medical imaging modalities, including CT scans, MRIs, and X-rays. These algorithms detect fractures, cardiovascular abnormalities, and lung nodules. Once the AI review is complete, the results are automatically transferred into the patient's EHR. This allows clinicians to view AI-generated reports alongside the patient's overall medical profile, ensuring that diagnostic insights are informed by clinical context.
AI-Related Security Concerns of EHRs
Although AI has redefined what EHR systems can achieve, it has also become a lucrative target for cybercriminals. A deeper look into these AI-specific threats reveals the scope of the challenges healthcare organizations must mitigate.
- Adversarial Machine Learning Attacks involve manipulating data to deceive AI systems, undermining their ability to make accurate predictions or diagnoses. For instance, by altering specific inputs, attackers might trick AI models into misdiagnosing a patient or recommending inappropriate treatments.
Impact: Imagine a healthcare AI model used to predict critical conditions, such as sepsis. With minor input changes, an attacker could prevent the system from generating alerts, delaying medical intervention, and potentially harming patient outcomes.
- Data Poisoning Attacks happen when malicious actors inject corrupted data into the training sets of AI models. This compromises the learning process, leading to unreliable predictions and inaccurate outcomes. When deployed in critical systems like EHR, this can lead to severe consequences, such as inappropriate treatment recommendations.
Impact: A poisoned dataset could deceive an AI system into predicting false results, like overstating mortality rates, causing unnecessary panic or misallocation of hospital resources.
- Membership Inference Attacks happen when attackers determine whether certain data points, such as sensitive patient information, were included in a model's training set. This could expose protected health information (PHI) and violate data privacy regulations like HIPAA.
Impact: Consider a malicious actor inferring the training data of a cancer prediction model. They could exploit this information to identify individuals with a specific medical condition, violating patient confidentiality.
- Model Vulnerabilities From External Sources. Organizations often adopt pre-trained AI models from external sources due to time and budget constraints; however, this introduces significant risks. Third-party models can include "backdoors," allowing attackers to trigger malicious outputs in specific scenarios.
Impact: An attacker could embed a backdoor into a pre-trained clinical decision-support tool. While the model functions normally in most cases, a deliberate trigger could produce inaccurate results, such as recommending unnecessary surgeries or delaying critical diagnoses.
Note: When discussing software development for healthcare companies, security is the number one priority. However, to make EHR systems secure, you need to distinguish the type of data being processed. The main concerns revolve around access to medical records and their sharing with third-party entities. Strict regulations, such as HIPAA in the U.S. and GDPR in the E.U., enforce robust controls to ensure patient data is used and shared responsibly. For general analytics or non-sensitive tasks, there is typically more flexibility and fewer restrictions. However, when utilizing commercial AI models from third-party providers, potential risks are reduced, allowing for more creative and innovative applications across healthcare functions.

Victoria Melnychuk
Other articles