AI in Hospital Management Systems

Healthcare systems around the globe are aspiring to achieve the quadruple aim. However, aging populations, the increasing prevalence of chronic diseases, and escalating healthcare expenses turn this aim into a challenge. The 2020 pandemic further complicates this task. It has also brought to light workforce shortages and disparities in healthcare access.
Along comes AI, promising to improve many aspects of modern medicine. Today, we will focus on the value it can bring to hospital management systems (HMS). This specifically concerns the area of patient care and administrative processes. We’ve conducted a thorough market overview to uncover the potential of AI and ML development in healthcare administration. We’ve also found exciting examples of AI clinic software that cater to patients' diverse needs.
We all aim for a future with accessible, efficient, and inclusive healthcare. So, let’s see if AI can deliver.
What is a Hospital Management System
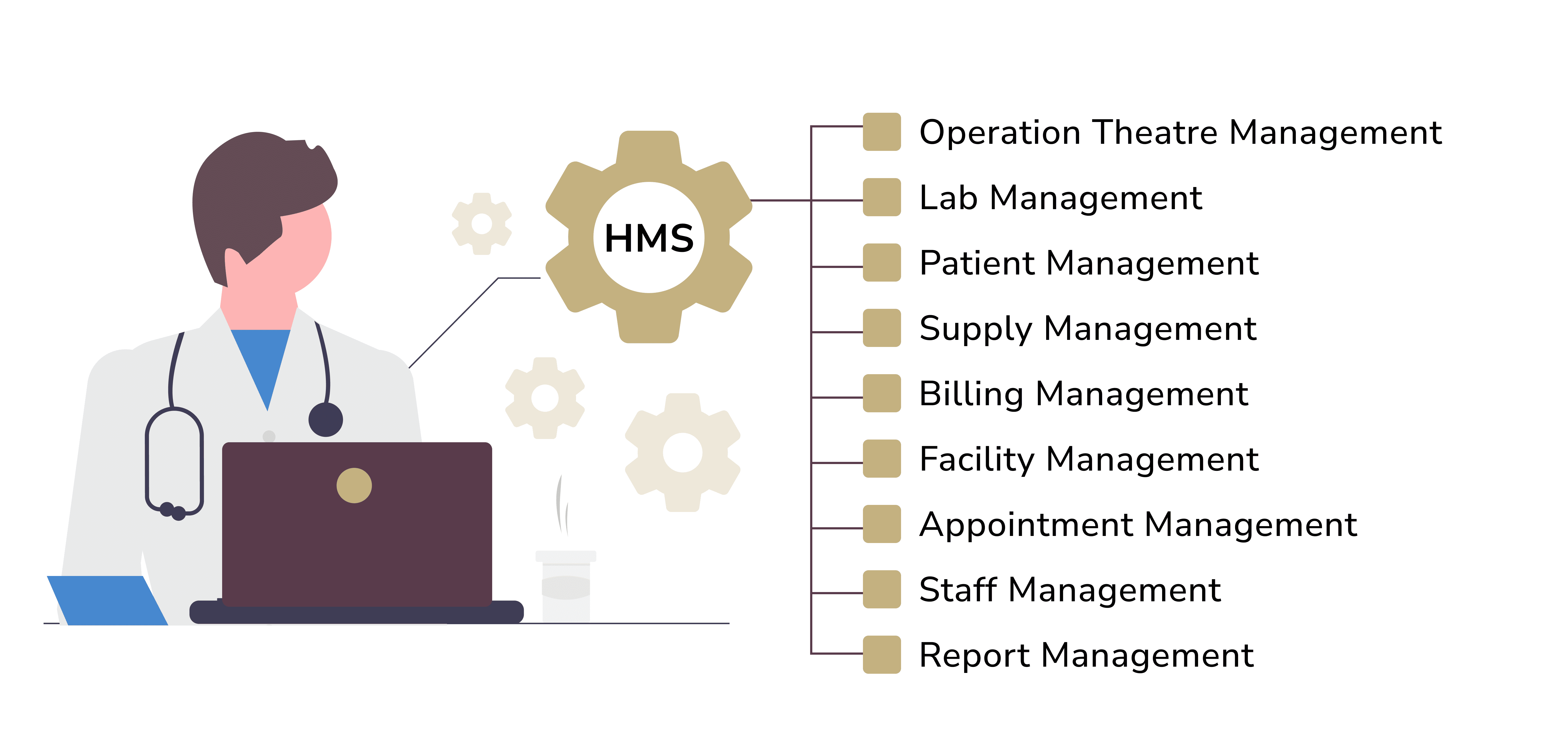
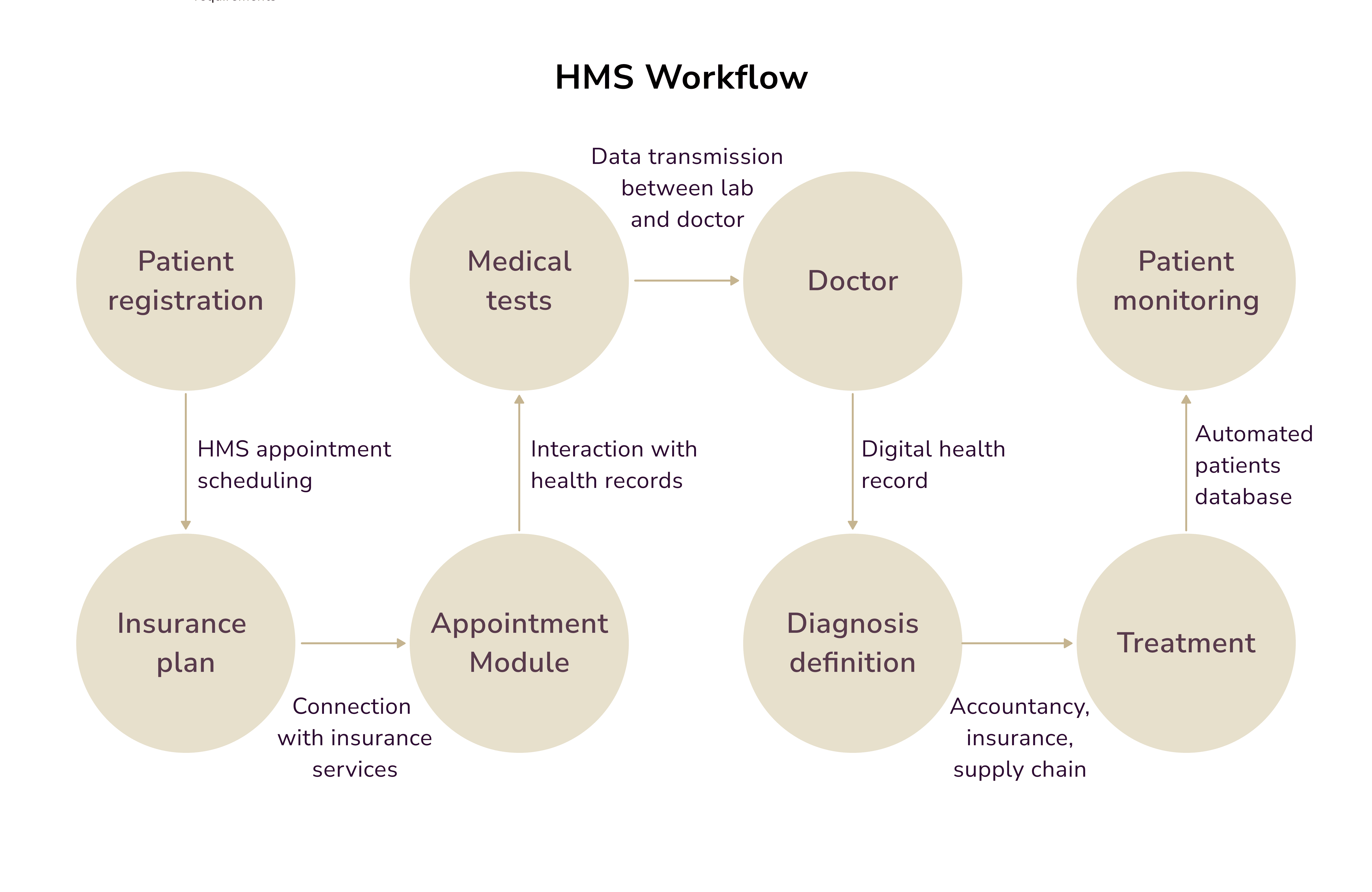
The hospital management system (HMS) is a computer system that handles healthcare-related data. It streamlines clinical, billing, financial, and administrative tasks inherent in hospital environments.
The 1960 launch of hospital database systems began an era of evolution. These systems have since become integral, merging with the hospitals' infrastructure, technologies, and software. Today, initiating healthcare processes can be as simple as using a mobile device or app. This puts control in the hands of patients before they even refer to healthcare providers.
Let’s explore the five main characteristics of HMS:
- A fundamental attribute of HMS is its ability to amalgamate various departments. It reshapes a hospital into a centralized platform where all operations take place. What does it encompass? Everything from scheduling and patient management to handling clinical data, billing, and inventory. This unification facilitates better communication among healthcare providers. Critical clinical information is always at hand, ready for collaborative decision-making.
- Patient management is another crucial aspect of HMS. The process entails consolidating medical records during admission, discharge, and registration. The HMS EHR lets clinicians quickly access patient information. This improves diagnostics and treatment planning.
- HMS automates billing processes, helping minimize human errors. The financial management of hospitals is intricate. It involves revenue cycle management, claims processing, insurance, claim preparation, and billing.
- HMS also encompasses inventory and supply chain management. The system ensures essential medical supplies are available. It also minimizes waste and costs.
- HMS often comprises analytics tools. So, admins can analyze large datasets to find patterns. This will improve patient outcomes.
Applications of AI in Hospital Management Systems
AI can handle many crucial duties in a hospital environment when implemented correctly. Here’s an example of a clinical and non-clinical use of AI in HMS:
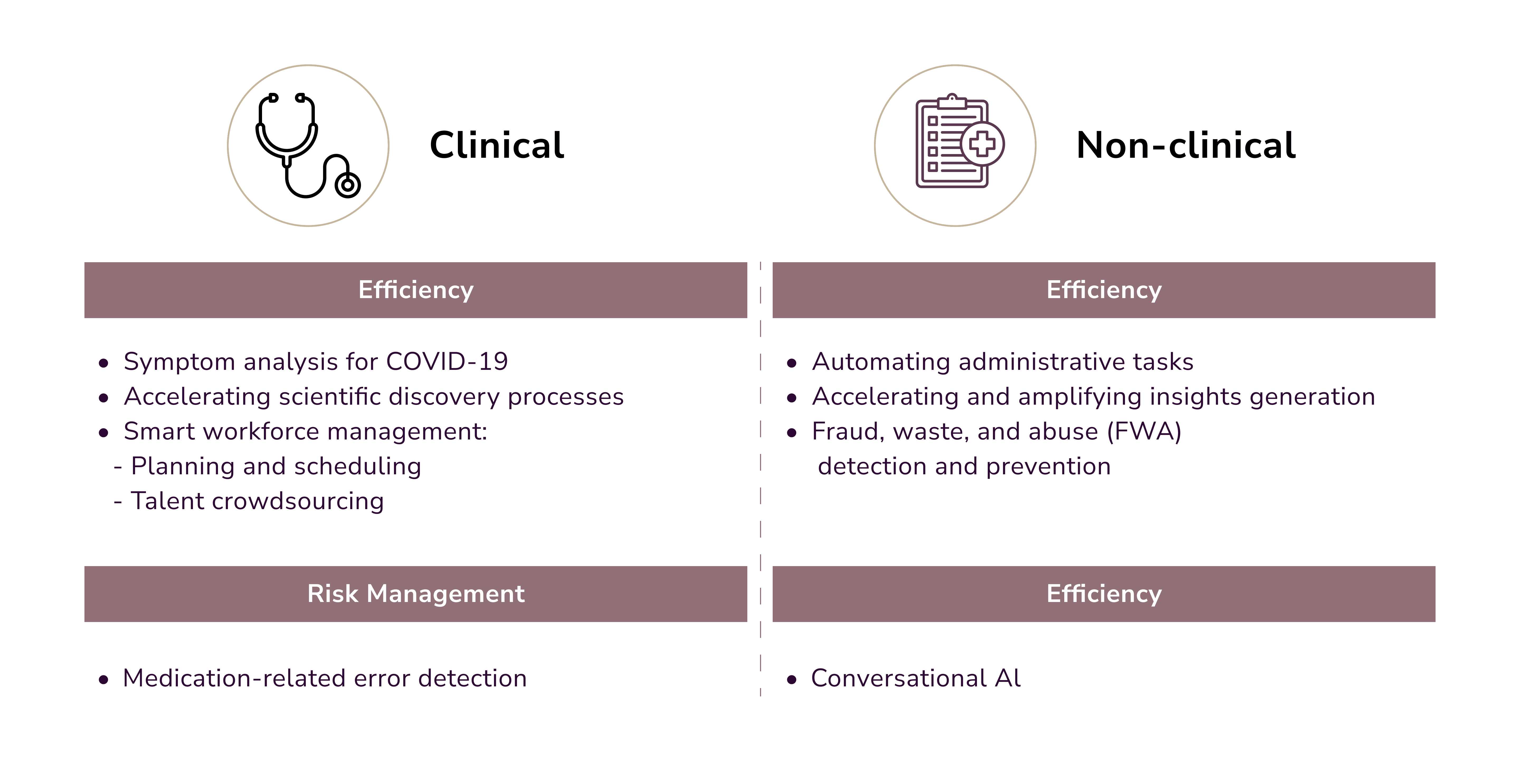
We’ll break down its use into four critical areas.
AI Healthcare Administration
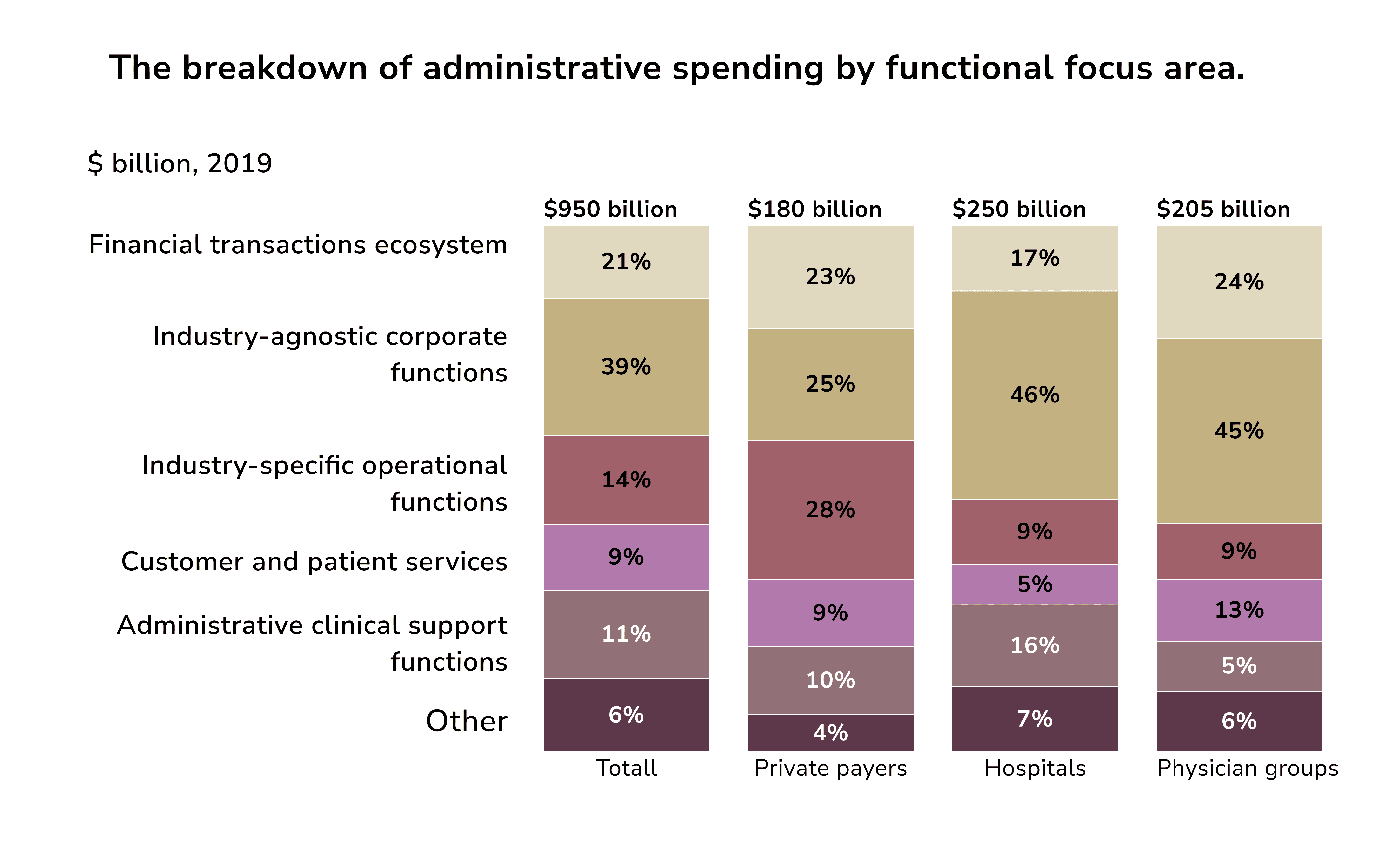
Administrative costs account for nearly a quarter of the $4 trillion spent on US healthcare. That leaves three-quarters for actual care. A critical question arises: How much of this spending is excessive? What strategies can we use to cut it?
Financial statements from payers and providers often lack the granularity. But that is precisely what can help distinguish between essential and non-essential expenses. Even with detailed data, it frequently doesn't match the framework of an organization's operations.
AI in healthcare administration can help with the following tasks:
- Data Management: AI algorithms excel at organizing EHRs. They quickly analyze them to provide access to crucial patient data.
- Workflow Optimization: AI optimizes workflows by automating and scheduling tasks. It improves staff allocation and appointment setting.
- Resource Allocation: AI in revenue cycle management helps save costs. It uses resources better. It makes the healthcare system more responsive to patient care needs.
Clinical Operations
Many have noted that AI’s rise mirrors the Gartner hype cycle. It began with a surge in “inflated expectations.” Then, there was a swift fall into the “trough of disillusionment” as the tech failed to meet those high hopes. However, a more measured use of AI and ML is unfolding now. It is genuine and brings value to patient care and clinical operations.
AI clinic software can help with the following tasks:
- Diagnostics and Imaging: ML algorithms excel at analyzing medical images, like X-rays, MRIs, and CT scans. They are trained on large datasets.
- Treatment Planning: AI clinical decision support systems help doctors customize treatment plans. They do this by using each patient's unique traits.
- Predictive Analytics for Patient Outcomes: AI can analyze past and current patient data. It can then predict health issues. This lets providers intervene early and prevent complications.
Patient Engagement and Experience
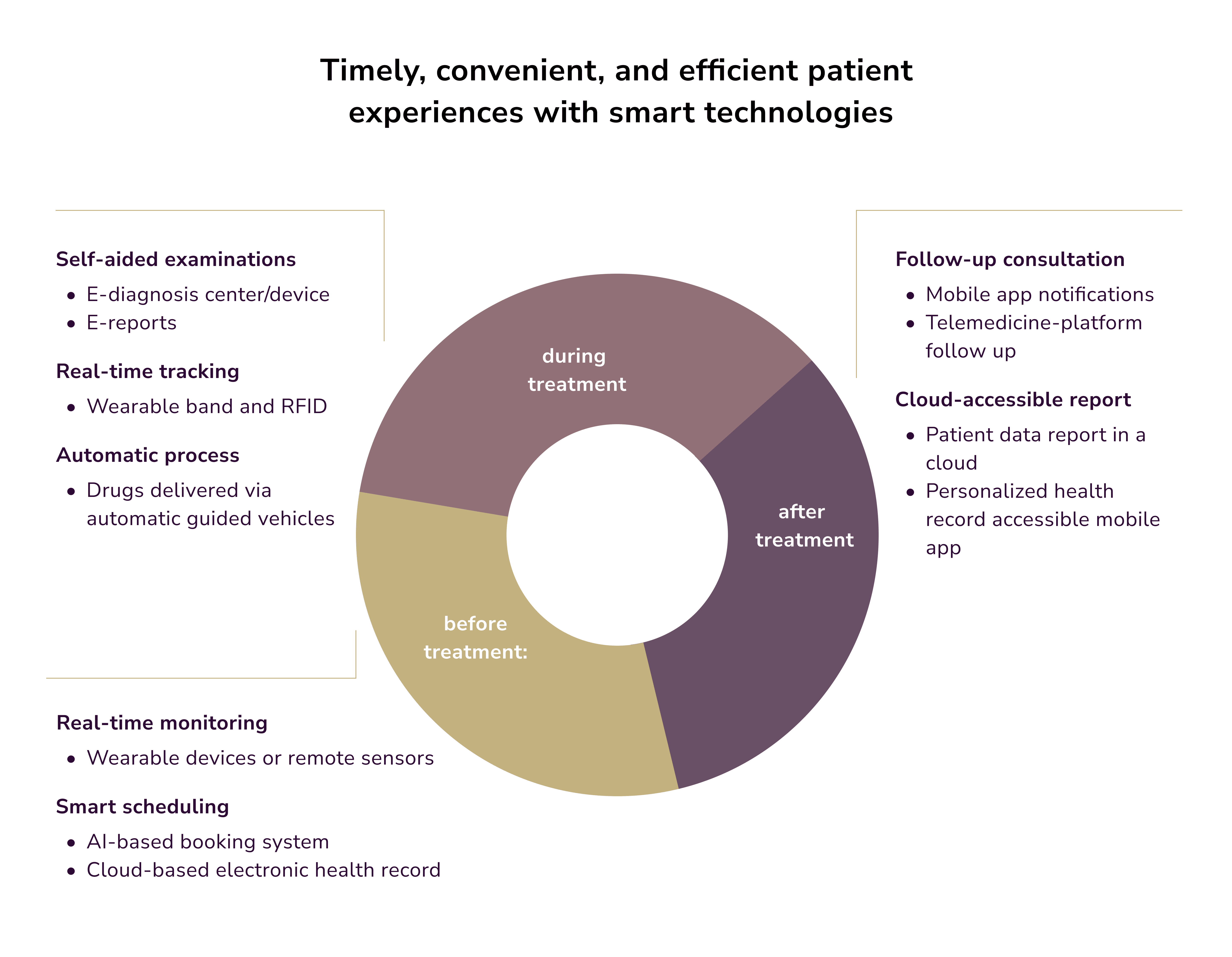
An often overlooked aspect of healthcare is the wait for the appointment. Kyruus Health says patients wait an average of 20.6 days to see a family doctor. Specialist wait times are even longer. In primary care, new patients wait 16 days for the third next available appointment (TNAA). Established patients wait about 12 days. While this area is often omitted, the WHO notes that patient involvement is integral to providing medical care.
AI-based mobile clinic management software can help with the following tasks:
- Personalized Healthcare: AI clinic software customizes treatment plans and sends reminders. It also provides health education materials for patient self-learning.
- Virtual Health Assistants: AI-driven, virtual health assistants, like chatbots, use NLP. They provide instant access to patients' medical info. Plus, they schedule appointments and offer essential healthcare guidance.
- Remote Patient Monitoring: AI-enabled remote monitoring solutions can finally free up nurses' time. Patients now actively manage their health conditions from home with just a smartwatch.
Nota bene: A patient information management system based on LLMs can aid in many tasks. It helps interpret clinical notes and navigate insurance claims. It also translates medical jargon into different languages. It captures nuances in expressions and dialects with great precision. This makes communication inclusive. 91% of Spanish-speaking parents in the US preferred translated discharge instructions for their children. This helps then enhance comprehension and adherence to care plans.
AI-Driven Decision Support Systems
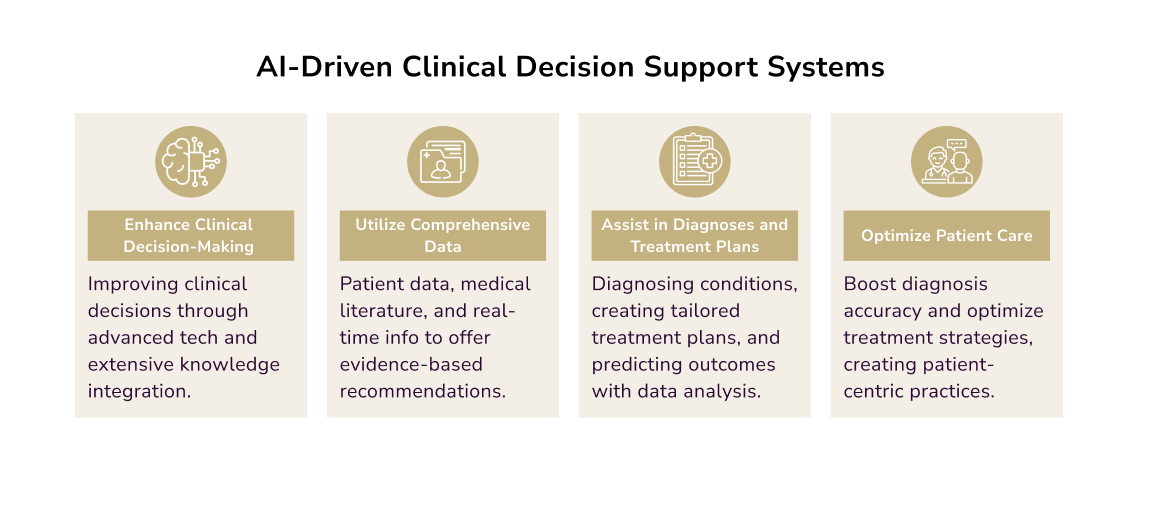
Clinical Decision Support Systems (CDSS) assist healthcare professionals in making complex clinical decisions. Since their 1980s introduction, CDSS have evolved into Intelligent Decision Support Systems (IDSS). They now integrate AI, offering insights and recommendations to improve decision quality.
An IDSS is designed to work like a human consultant. It gathers and analyzes data to help decision-makers find and solve problems. It also evaluates potential solutions. The AI closely mimics human thought. But it can process and analyze data better than any human.
IDSS in healthcare can help with the following tasks:
- Clinical Decision Support: AI software for clinic decisions helps complete multiple tasks. These include diagnosis, treatment strategies, and patient outcomes prediction. Ultimately, it transforms patient care into more informed, efficient, and patient-centric practices.
- Operational Decision Support: AI clinic management software also analyzes extensive datasets. These include resource utilization, staff scheduling, and workflow efficiency. It then identifies patterns and trends for informed decision-making.
How does AI-Powered Hospital Management Software Enhance Patient Care?
Focusing on patient care, we researched five significant areas in which AI already makes an impact.
Enhanced Communication
Healthcare professionals cannot overstate the importance of real-time data sharing. Data analytics helps manage drug therapy (identify side effects, drug interactions, and toxicities). Nurses put orders directly into the EHR, which talks to the pharmacy. Medications are dispensed by machines similar to ATMs, following thorough safety checks. Nurses then scan the patient's armband and medication with barcodes. This ensures they match and receive the necessary drugs.
Personalized Treatment Plans
A personalized approach to patient treatment yields better outcomes and minimizes adverse effects. One way AI can ensure that is through data:
- Genetic Profiling: AI algorithms evaluate genetic information. This helps assess a patient's likelihood of certain diseases and response to medications. This insight is vital for crafting personalized treatment plans.
- Biomarker Validation: AI is essential to finding and confirming biomarkers. It can also help ensure treatments are tailored to an individual's unique physiology.
- Clinical Trials: AI improves the selection of clinical trial participants. Genetic and clinical data are used to make accurate choices. It increases trial effectiveness and efficiency. It also lowers costs and time.
Reduced Diagnostic Errors
A study in BMJ Journals revealed worrying stats on misdiagnoses and their effects. Here are some crucial insights:
- A staggering 75% of the harm from misdiagnosis is due to vascular issues, infections, and cancers.
- Fifteen high-risk diseases account for nearly 51% of severe harmful outcomes from misdiagnoses.
- Of these, 371,000 die from medical mistakes. Another 424,000 are disabled.
- The overall error rate across different diseases is 11.1%.
AI-powered tools can serve as second-opinion resources for medical centers. They can assist in validating diagnoses and reducing misdiagnosis risks. This support is invaluable in complex cases or rare diseases where expertise may be limited.
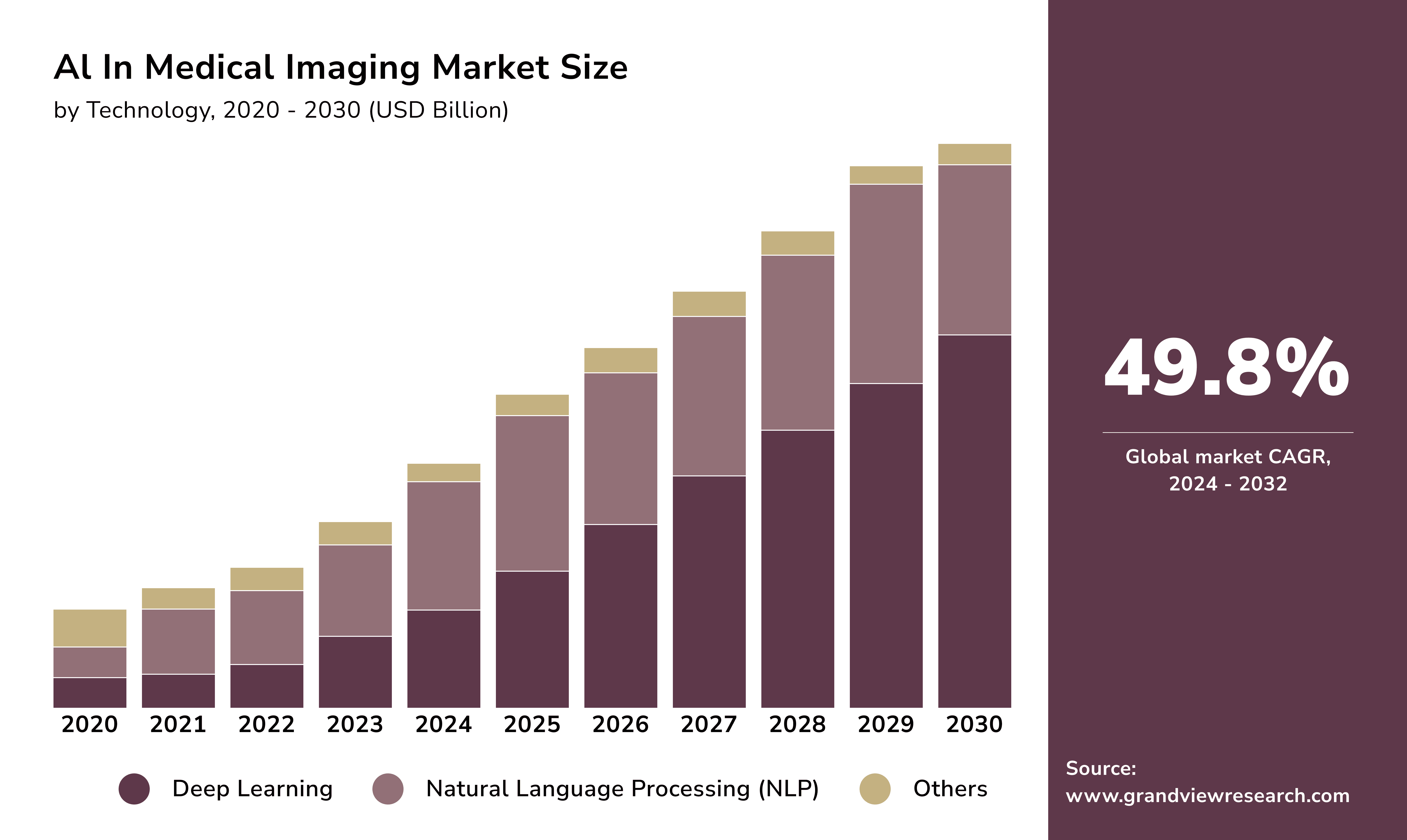
Nota bene: ML is increasingly used in computer vision, CAD, and image processing to help diagnose diseases. The use of various imaging technologies has greatly advanced medical imaging. These include multi-slice computed tomography (CT), positron emission tomography (PET), tomosynthesis, magnetic resonance imaging (MRI), tomography, and diffuse optical tomography.
The Role of Deep Learning in Diagnostics
Recent progress in DL pushed for robust predictive model development capable of early disease detection. These algorithms surpass traditional ML techniques due to their
- extensive data analysis capabilities
- automated feature extraction
- exceptional accuracy.
Evidence suggests that DL algorithms outperform ML in managing large datasets. They also surpass human accuracy, particularly with image processing. This has drawn much interest in medicine, especially diagnosing with medical images. Examples of such algorithms include
- recursive neural networks
- deep belief networks (DBNs)
- deep autoencoders
- deep Boltzmann machines, and more.
A notable tool in medical data analysis is the RAGCN. It is a region aggregation graph convolutional network. This tool uses graph convolutional networks (GCNs). It integrates and simplifies data from different parts of an image. It analyzes medical images, like CT and MRI scans. These often have multiple regions of interest (ROIs) that need separate analysis. For instance, scientists can now use CNNs and GCNs to determine bone age. They can use CNNs for feature extraction and GCNs for identifying critical bone locations.
The LAPNet model uses a pyramid design to extract key features from images of different sizes. It emphasizes regions prone to lesion formation through an attention mechanism. This approach assessed diabetic retinopathy. A large dataset of medical images trained LAPNet to identify lesion regions.
Predictive Analytics for Early Intervention
Some researchers use explainable AI to gather data for disease prediction or diagnosis. One example is SHapley Additive exPlanations (SHAP), which identifies the most critical factors. Meanwhile, the generation of synthetic medical images fostered the advancement of generative models. Particularly generative adversarial networks. These images can enhance current data, such as those related to lung diseases. These networks improve the accuracy of the results. Both methods complement each other well and can enhance model efficiency.
AI and predictive analytics play a life-saving role in sepsis detection. A good example is HCA Healthcare's use of S-P-O-T. It stands for Sepsis Prediction and Optimization of Therapy. This algorithm leverages clinical data to detect sepsis and ensure rapid, timely intervention.
The PARAllel predictive MOdeling (PARAMO) platform is a significant player in healthcare analytics. It utilizes EHRs to boost predictive modeling processes across patient groups. This comes in handy during healthcare crises. This software significantly reduces modeling task computation times through parallel job processing.
Enhancing Chronic Disease Management
The CDC reports that 60% of U.S. adults have chronic conditions. Of these, 40% have multiple chronic illnesses. AI in healthcare administration enables remote monitoring of chronic patients. They provide real-time feedback and alerts to healthcare providers. Wearable devices and apps allow continuous data collection. They let clinicians track patients’ vital signs and symptoms.
A recent Time article discusses medical digital twins. This tech lets doctors examine digital replicas of patients’ hearts. They can then apply suitable, tested treatments. A prominent example is Mare Nostrum, a Barcelona-based supercomputer. It has a virtual model of a patient’s heart and 100 million patches of simulated cells. This digital twin heart tests treatments, from drugs to implants. Similar projects focusing on digital twin hearts are being developed globally.
How is an AI-Powered Hospital Management System Helpful to Healthcare Professionals?
US healthcare organizations continue to face challenges due to an ongoing nursing shortage. The shortage has cut healthcare services. It has also increased staff burnout and mental health issues.
McKinsey has tracked trends in the nursing workforce. It gathered data on nurses’ plans to leave their jobs. It also looked at the factors influencing their decisions. As of March 2023, 45% of nurses in the U.S. planned to leave their jobs. That's about 2 million of the 4.2 million employees. The main reasons cited were “feeling undervalued” and having an “unmanageable workload”. Increasing workload has consistently been a significant factor driving nurses' decisions to leave.
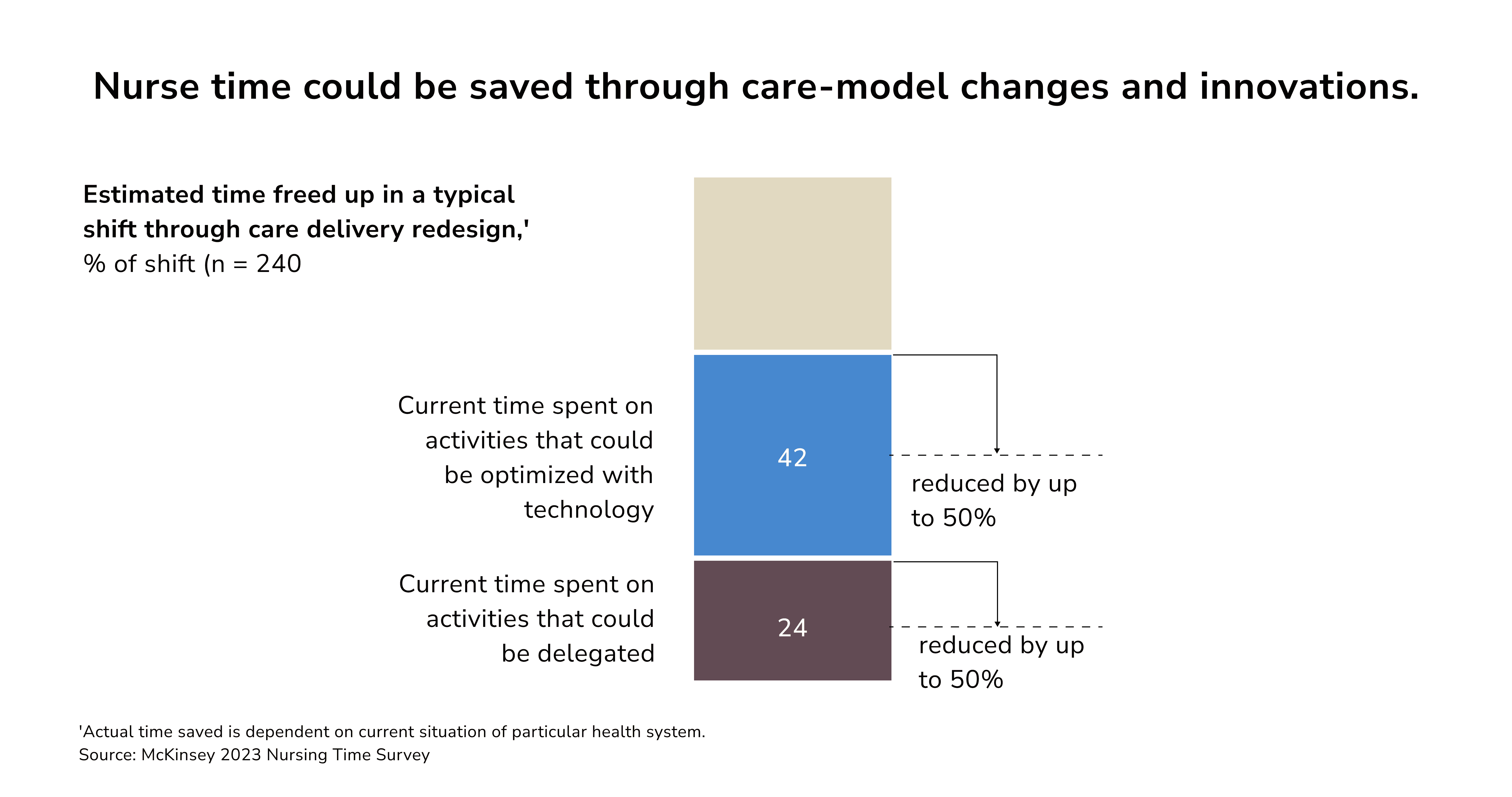
AI healthcare management aims to help providers deliver high-quality care and reduce burnout.
Remote Patient Monitoring
Many companies have developed AI-driven remote patient monitoring systems to check vital patient signs. They include heart rate, blood pressure, and oxygen levels.
What exactly are these devices?
- Wearable devices and sensors allow real-time tracking of vital signs. They help healthcare providers to detect major diseases early and manage chronic conditions. They support continuous monitoring, minimizing hospital visits, and improving patients’ quality of life.
- EHR and patient portals give patients access to their health data. These technologies empower patients to control their healthcare. They enable direct communication with their medical team. They also ensure cohesive care across providers.
- Mobile health apps offer tailored info and monitoring. They meet patients’ needs and preferences.
- Telehealth and secure messaging improve communication between providers and patients. They foster trust and transparency.
- Social media platforms let patients engage in their care. Users can share experiences with others facing similar health issues. They can also improve interactions with healthcare professionals.
Remote Consultations
The COVID-19 pandemic showed the value of advanced digital technology. It enabled safe-distance patient care. The pandemic sped up the use of teleconsultations. It offered a chance to restructure the general practitioner’s office operations.
A notable example is the OneRemission app. It assists cancer survivors, cancer patients, and their support network. OneRemission also includes a 24/7 AI chatbot. It answers questions about cancer care and post-treatment lifestyle.
Another great example is Teladoc Health. This platform serves many medical needs. It covers routine issues like the flu and respiratory infections. It also addresses chronic severe conditions, such as cancer and heart failure.
Making Sense of Mountains of Data
Health data has grown tremendously. But, 97% remains untapped. This offers a gateway to boost the health system. AI-based clinic software turns unstructured data into clinical insights. It improves data flow to support optimal care beyond the clinic. Data-driven digital solutions can thus make healthcare more sustainable, resilient, and effective.
AI excels at processing vast datasets. It quickly spots patterns that would challenge humans. Without AI, healthcare admins and IT pros would have to compile this data manually. But they often lack the time or skills for such a monumental task.
Patient Engagement and Adherence
Improving patient engagement and adherence represents the so-called "last mile" challenge in healthcare. It denotes the final hurdle between suboptimal and successful health outcomes. See, when patients engage in their own care, it improves outcomes.
This area is increasingly being addressed through big data and AI. A new healthcare management AI trend is choice architecture. It uses real-world evidence to influence patient behavior subtly. Clinic software can improve recommendations by using data from various devices. These include EHR systems, biosensors, smartwatches, smartphones, and chatbots. It will compare patient data with effective treatment pathways for similar demographics. These tailored recommendations can assist all parties in the healthcare ecosystem. From providers, patients, nurses, and call center agents to care coordinators.
AI-Powered Healthcare Management System Examples
Many healthcare orgs have created AI clinic software to enhance patient care delivery.
- University of Pittsburgh Medical Center has developed the Concierge. This AI-driven system allowed UPMC to improve patient outcomes and reduce costs. The solution uses predictive analytics to find at-risk patients. It aims to prevent readmissions and complications. This approach has led to a 30% decrease in hospital readmissions and a cost reduction of $2,200 per patient. Additionally, it has shortened hospital stays and boosted patient satisfaction.
- Cleveland Clinic created an AI-powered system named CLEVELAND. It has expedited the process of matching patients with clinical trials. The system extracts data using NLP to find suitable clinical trials for patients. This has significantly reduced the matching time from months to mere minutes. The system has also increased the enrollment of patients in clinical trials.
- University of Chicago Medical Center has adopted a predictive analytics system. It employs ML algorithms to detect patients at risk of sepsis. This initiative has cut sepsis deaths by 30%. It shows the potential of AI healthcare management systems to improve patient care.
- Stanford Health Care deployed an NLP system to scrutinize clinical notes. This helped Stanford improve diagnostic accuracy. This system has cut diagnostic errors by 26%. It shows that AI can improve decision-making.
- Geisinger Health System is implementing an AI-powered clinical decision support system. It assists doctors in selecting optimal treatment plans. This system has cut healthcare costs by $11 million a year. It shows the savings possible with AI in healthcare administration.
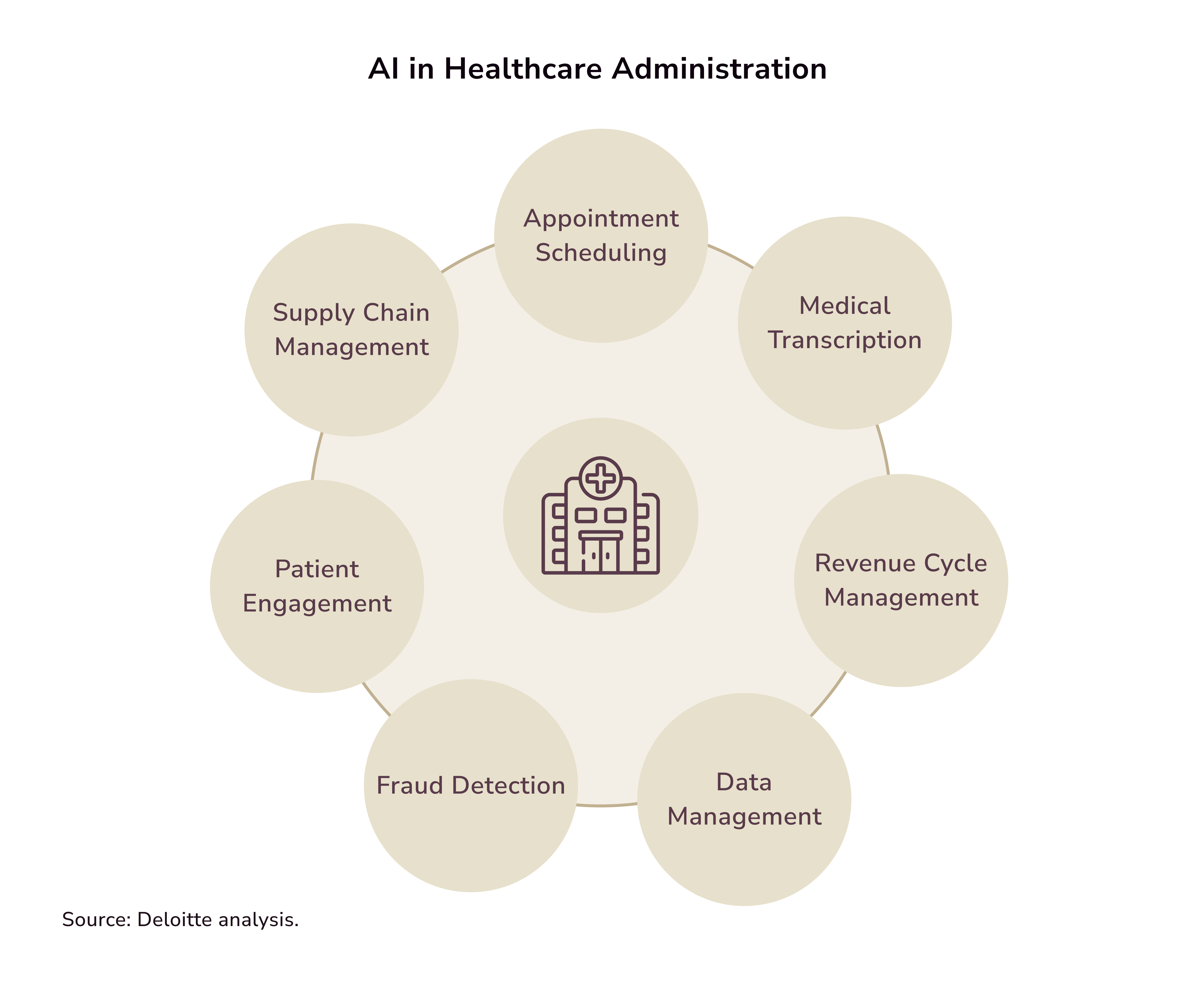
AI in Healthcare Administration
The burden of admin duties on clinicians is immense, especially after COVID-19. This area of healthcare often goes unnoticed by those outside the industry. Here's why this matters:
- 25% of U.S. healthcare spending goes to admin tasks. Implementing automation could potentially reduce this expenditure by 25-30%.
- Clinician burnout is a growing problem in health systems, especially in the US. Over 90% of clinicians blame excessive admin work for their burnout.
- The lack of smooth information flow has fragmented healthcare. It is now divided into entities like providers, payers, and the government. This fragmentation leads to misaligned incentives and minimal integration.
NLP-based solutions are well-suited for simple tasks like prescription refills and appointment scheduling. AI systems automate scheduling, billing, and patient records. This lets healthcare workers focus on quality care.
How to Improve Patient Satisfaction through Administrative Practices (Use Cases)
Enhancing patient satisfaction is a crucial focus for clinics. Let’s take a look at their progress so far.
Enhancing Communication Channels
Johns Hopkins Hospital in Maryland partnered with GE to improve hospital visit efficiency. This strategic move has led to faster hospital visits using AI-driven predictive analytics. Their predictive AI tool also solves operational problems. It improves the patient experience by reducing delays and streamlining hospital check-ins.
Personalizing Patient Experiences
IBM and Cleveland Clinic have formed another strategic alliance. They harnessed AI to transform how they personalize healthcare plans for their patients. Their advanced system lets the clinic analyze vast data sets. AI-driven insights help Cleveland Clinic refine treatment plans and boost diagnostic precision. This ultimately results in enhanced patient outcomes.
Reducing Wait Times
Ciox Health has created an AI clinic manager software. It will manage health data and workflows. The focus is on using ML to improve health data management and exchange. Ciox Health aims to ensure that doctors can access crucial data in a timely manner. This will help them make informed decisions. The initiative truly showcases the potential of AI. It says that health data exchange could improve patient care.
AI’s Role in Smart Hospitals
The technological advancements driving smart cities similarly underpin the development of smart hospitals. Edge computing, for instance, processes data closer to its origin. Whether it be from a patient’s bedside or a diagnostic device. It thus minimizes latency and allows for immediate response. In critical care settings like ERs and ICUs, quick decisions are vital.
Consider how AI optimizes urban functions, like managing traffic in smart cities. Similarly, it can alter hospitals. AI can handle patient flow, forecast demand, and optimize staffing. Predictive analytics help hospitals foresee healthcare needs. This fosters a proactive approach to patient care.
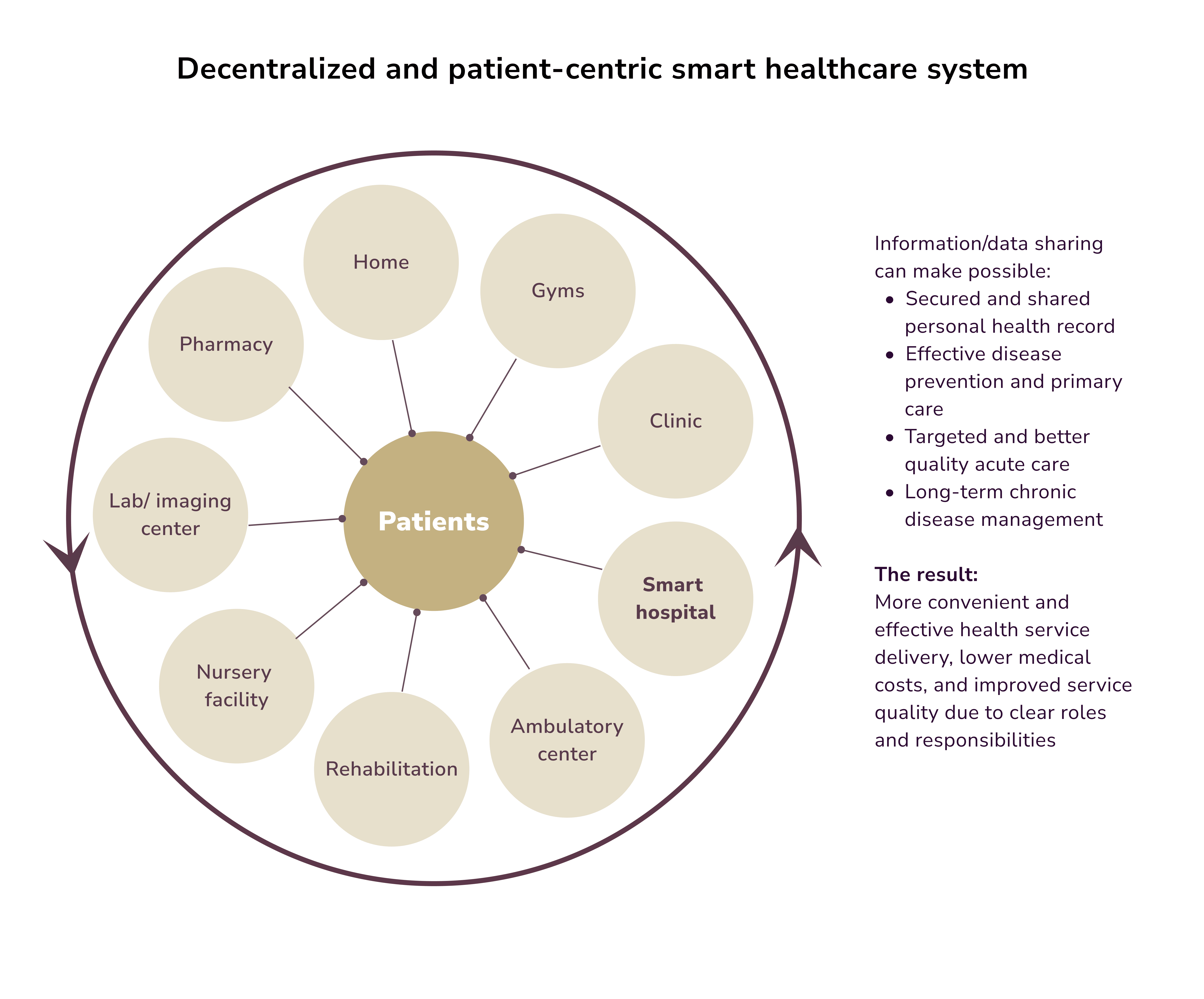
Harnessing AI in healthcare can help craft a comprehensive, integrated, intelligent health system. This system can rely, for instance, on layers of data integration and analysis. They will be connected by a data backbone. Each data layer will compare patients' data to their baselines and similar cohorts. Their personalized data cloud will feed into it. The system can, from this, create targeted interventions. It will refine care strategies for each patient based on learned outcomes.
Embracing the Future of Healthcare Management with AI
We'd also like to outline key upcoming trends:
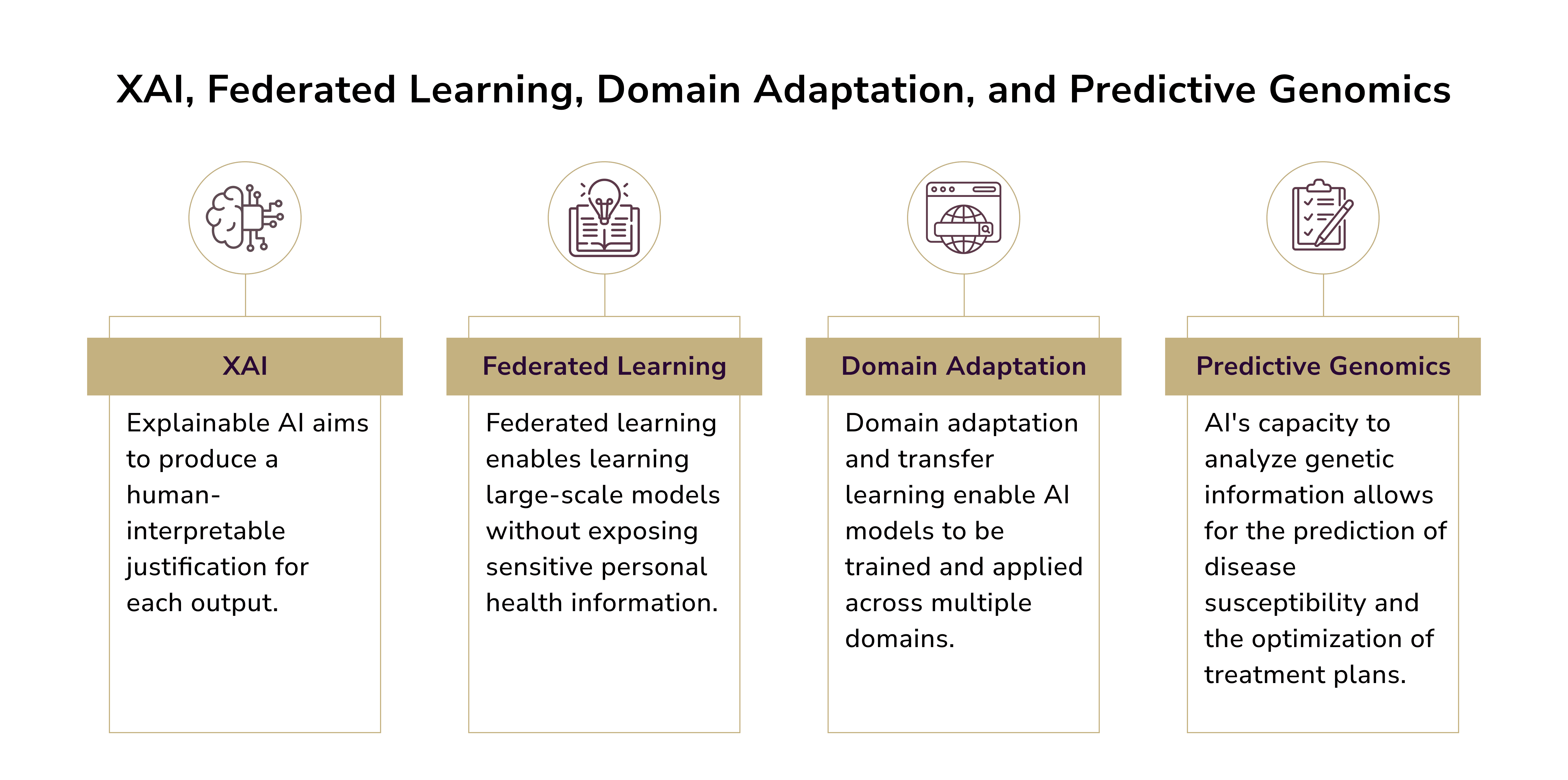
- Explainable AI (XAI). In healthcare, there is a push for more transparent, understandable AI systems. This is where XAI comes into play. It aims to clarify complex AI models. This will help healthcare providers understand how AI algorithms make decisions. Such transparency is vital in clinical settings.
- Federated Learning. This method trains ML models across many devices or servers. It does so without sharing raw data. So, different hospitals and research entities can safely enhance AI models. They can do this while keeping patient data secure. Federated learning protects privacy and enables large-scale collaboration. It will lead to more secure AI in healthcare research.
- Predictive Genomics. AI can analyze genetic data. It can predict disease risk, optimize treatments, and help create targeted therapies. Predictive genomics can help create personalized treatments. It can alter our understanding of genetics in health and disease.
- Domain Adaptation. Domain adaptation is a tech that creates a modified image for different domains. It aims to improve the AI's reading accuracy with varied image distributions in GI endoscopy and medical image analysis.
Want to explore AI in healthcare further? Click here for details on custom software development for healthcare companies.

Victoria Melnychuk
Other articles